Before he was suddenly fired, FBI Director James B. Comey gave an impassioned but unconvincing defense about his probe into Hillary Clinton’s private email server a week before the presidential election. Although many believe his investigation may have affected the outcome of the election, he told a Senate panel he has no regrets despite feeling “mildly nauseous.’’ [1]
When President Trump inexplicably told Comey, “You’re fired,” more questions arose about the future of the FBI investigation into Trump’s campaign ties to the Russian government to steer the outcome of the 2016 presidential election.
I wonder if Russian President Vladimir Putin feels “mildly nauseous’’ for his meddling, too?
Medical Meddling
The same accusation can be made of the medical meddling in spine care that has now led to a “national scandal”[2] consisting of thousands of deaths in the opioid painkiller pandemic and a wake of disability from hundreds of thousands of failed back surgeries that fly in the face of new research and guidelines.
Thomas Frieden, MD, director for the CDC, mentioned, “The opioid epidemic is devastating American families and communities.”[3] Today there are 13 million users, 2 million abusers, and 165,000 have died since 1999 from opioid overdose.[4]
Dr. Frieden commented about “the burden of dangerous drugs.” Considering one in 20 U.S. adults is now addicted to prescription narcotics, he said physicians have supplanted “drug pushers on the street corners” as the most important suppliers of illicit narcotics.[5]
More shocking facts: every 19 minutes, someone in the United States dies from an unintentional prescription drug overdose.[6] Today one in 12 Americans can say they know someone who died from a prescription drug overdose. No other disease can make that claim.[7]
I wonder if the pain management clinics in cahoots with Big Pharma who orchestrated this opioid epidemic are “mildly nauseous” with the addiction, deaths, and disability they’ve created?
Can we tell these medical meddlers and drug peddlers “You’re fired” for creating the biggest drug addiction crisis our nation has ever seen?
Friend at FOX
The only medical reporter who has publicly accepted blame for the opioid pandemic is Dr. Marc Siegel at FOX News who openly admitted primary care providers were the cause of this opioid crisis, aka, Pharmageddon.
Dr. Siegel was extremely forthcoming when he blamed the opioid epidemic on his own colleagues and pharmacists; he also admitted MDs have only 9 hours of education on “back,” supporting the notion MDs are inept in musculoskeletal disorders and back pain in particular.
Maybe Dr. Siegel should tell his primary care colleagues, “You’re fired,” for creating this opioid crisis. He might also admit they should never have accepted these chronic pain patients in the first place since they are unschooled in musculoskeletal disorders that constitute 70% of opioid prescriptions.[8]
Dr. Siegel was painfully honest when he said, “We’re getting a growing awareness of two things: the abuse of back surgery and the abuse of opioids… Let’s replace [them] with things that work – heat, weight loss, exercise, physical therapy, acupuncture, chiropractic.”[9]
If only more MDs thought this way…
Click on arrow to begin video.
Dr. Marc Siegel on FOX News after his appearance at the NPC.
Approaching the Tipping Point
Just as a string of events led to Director Comey’s firing, we’ve also seen a timeline of recent events in spine care that I wish every potential spine surgery patient knew that would lead to the firing of MDs parading as spine experts.
If our profession had an effective PR mechanism in the earned media, this information could substantially change our image as reformers, reveal the incompetence of MDs in MSDs, and to boost the public’s understanding of this medical spine care/opioid travesty.
Take a look at this string of important events:
- On February 14, 2017, spinal manipulative therapy (SMT) was listed as a front-line treatment by the updated American College of Physicians (ACP) guidelines that recommended no drugs, not even OTC, epidural shots or surgery. ACP recommended SMT, massage therapy, yoga, tai chi and other CAM treatments.
By coincidence, two other news releases concerning the poor performance of drugs for back pain and sciatica were released shortly afterwards condemning pain pills as worthless:
- On March 17, 2017, television news reported Ibuprofen can increase heart attack risk by 31%.
- On March 23, 2017, another news release from the New England Journal of Medicine found Pregabalin (Lyrica) for acute and chronic sciatica was no better than placebo.
On April 11, 2017, another shocking study was released in JAMA:
- “Association of Spinal Manipulative Therapy With Clinical Benefit and Harm for Acute Low Back Pain Systematic Review and Meta-analysis” recommends spinal manipulation as a first-line treatment for LBP.
- In the same edition, Richard Deyo, MD, MPH, authored an editorial, “The Role of Spinal Manipulation in the Treatment of Low Back Pain,” published in conjunction with the original investigation. (You might enjoy my response to his editorial, “Bones of Contention”)
- Also on April 11, NPR aired a recap: “Spinal Manipulation Can Alleviate Back Pain, Study Concludes.”
- A few weeks later on May 1, 2017, Aaron E. Carroll, MD, wrote in the New York Times an insightful analysis, “For Bad Backs, It May Be Time to Rethink Biases About Chiropractors.” (You will enjoy my response to him)
Finally, an honest MD willing to admit to his bias about chiropractic care!
“A physician like me might suggest any number of potential treatments and therapies. But one I never considered was a referral for spinal manipulation. It appears I may have been mistaken. For initial treatment of lower back pain, it may be time for me (and other physicians) to rethink our biases.”
Wow, if we could get the other half million MDs to admit to their biases, too, it would explain to the public and press that the medical war against chiropractors was unwarranted and also had collateral damage in terms of patients addicted to opioids and suffering from failed back surgery.
It would also helpful if MDs, like Dr. Siegel, admitted to their lack of training in spine-related disorders as Dr. Rick Deyo wrote:
“Calling a physician a back-pain expert, therefore, is perhaps faint praise—medicine has at best a limited understanding of the condition. In fact, medicines’ reliance on outdated ideas may have actually contributed to the problem.”[10]
Scott Boden, MD, currently director of the Emory Orthopaedic and Spine Center in Atlanta, has also confessed, “Many, if not most, primary care providers have little training in how to manage musculoskeletal disorders.”[11]
Unfortunately, MDs will not fire themselves or admit their bias and incompetence. If we don’t inform the public and press, no one will.
Like the Russian investigation that may open up a can of worms exposing the White House to public ridicule and legal action, if word got out via the news media of the incompetence and malpractice of MDs who have created this back pain fiasco, it would expose them all to lawsuits for lack of informed consent and proper referral to nondrug, nonsurgical providers like chiropractors.
Indeed, such an admission could be a “bigly” blow to the medical spine care industry and would make for a huge shift in the marketplace, and one chiropractors should fill.
New Guidelines
Previous spine studies supporting the shift in spine care have rarely been brought to public attention by MDs or medical reporters. The foremost study ignored was the comprehensive 1994 AHCPR Guideline #14 on acute low back pain in adults that should have revolutionized spine care, but was sabotaged by the North American Spine Society (NASS) with former Rep. Newt Gingrich (R-GA) leading the charge on Capitol Hill to de-fund the agency.
Ironically, years later the NASS released its own guidelines supportive of conservative care:
- In 2007, the NASS published Diagnosis and Treatment of Degenerative Lumbar Spinal Stenosis. This study[12] provides Level IV therapeutic data suggesting that distraction manipulation and neural mobilization may be beneficial in the treatment of lumbar spinal stenosis.
- In 2010, the NASS released “Contemporary Concepts in Spine Care: Spinal Manipulation Therapy for Acute Low Back Pain” recommending spinal manipulation—5 to 10 sessions over 2 to 4 weeks—should be considered before surgery.
- In 2012, the NASS also published Clinical Guidelines for Multidisciplinary Spine Care Diagnosis and Treatment of Lumbar Disc Herniation with Radiculopathy that found “patients with lumbar radiculopathy due to lumbar disc herniation, 60% will benefit from spinal manipulation to the same degree as if they undergo surgical intervention. For the 40% that are unsatisfied, surgery provides an excellent outcome.”
Wouldn’t it be great if the public and press knew of these NASS recommendations vindicating the value of chiropractic care?
Other reports have also debunked the effectiveness of other medical methods:
- In November, 2014, the Mayo Clinic published a systematic review of 33 studies from around the world that agree “bad discs” are commonplace among pain-free people, equivalent to grey hair, a natural part of the aging process and not an indication for surgery.
- In 2014, the FDA published FDA Drug Safety Communication that found off-label use of epidural steroid injections (ESI) to be no better than placebo, sometimes dangerous such as loss of vision, stroke, paralysis, and death, and ESI have never been approved by the FDA for back pain.
- In 2015, The New York Times published “Physical Therapy May Not Benefit Back Pain” that reported “Physical therapy may provide little relief for recent-onset low back pain.”
- In 2015, a study in Spine concluded: “The majority of the study population was on Chronic Opioid Therapy after fusion. COT was associated with considerably worse outcomes. The poor outcomes of this study could suggest a more limited role for discogenic fusion among WC patients.”
Stop Spine Surgeries
Neurologist Scott Haldeman, MD, DC, PhD, a world-renown multi-disciplinary researcher from UCLA, confirms that “virtually all guidelines” on spine care now advocate conservative care first:
“The paradigm shift has already taken place. Non-surgical, non-invasive care is already the first choice for treatment for spinal disorders in the absence of red flags for serious pathology in virtually all guidelines.”[13]
Unfortunately, his message has fallen on deaf ears among surgeons despite the mounting evidence that spine surgeries are most often unnecessary, lead to opioid dependency/abuse, conservative care is preferable in most cases, and a waiting period often helps.
On May 4, 2017, a new study found patients scheduled for lumbar spine surgery who were reviewed by a multidisciplinary team significantly deterred unnecessary and costly surgeries.
The study admits lumbar spine surgery has increased eight-fold over the past 30 years and a “troubling number of randomized controlled trials showing overall outcomes to be no better than those seen with nonoperative care.” These cases were reviewed by a broad range of specialists instead of just following the recommendation of a single surgeon.
Vijay Yanamadala, MD, said in presenting the study at the American Association of Neurological Surgeons 2017 Annual Meeting, “When non-surgeons are empowered to make decisions, nearly 60% of patients who were recommended surgery were found to have nonsurgical options.”
Notably missing is any mention of chiropractic care in this study. The study mentions “a multidisciplinary conference involving physiatrists, anesthesiologists, pain specialists, neurosurgeons, orthopaedic spine surgeons, physical therapists, and nursing staff,” but no mention of DCs. Apparently chirophobia still infects the ANNS.
This omission of DCs comes as a surprise considering a 2013 “Military Study: Low-Back Pain Relief with Chiropractic Care” featured the benefit of adding chiro care to medical spine care.
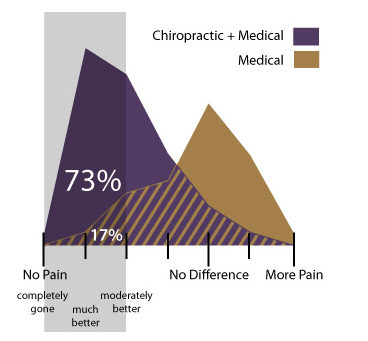
This low-back pain study led by Christine Goertz, DC, PhD, from the Palmer Center for Chiropractic Research, found 73 percent of those who received standard medical care and chiropractic care rated their improvement as pain “completely gone,” “much better” or “moderately better.” In comparison, 17 percent of participants who received only standard medical care rated their improvement this way.
More evidence of the low need for disc surgery emerged in May, 2017, from a study in Spine reporting the natural reduction of herniated discs:
“15% to 93% of herniations reduced in size or disappeared without surgery, with higher rates typically reported at longer follow-up periods… For patients to understand that some MRI findings can improve or resolve naturally can be useful information to facilitate patient-centered, informed treatment decisions during the course of an episode of LBP or sciatica.”[14]
Another article from Down Under reflected the same sentiments to monitor/delay possible spine fusions. On April 26, 2016, the Medical Journal of Australia InSight newsletter published, “Spinal Fusion Surgeries Questioned,” that was painfully clear on the need to stop the tsunami of back surgeries:
“Spinal fusion surgeries for chronic low back pain are on the rise, despite the lack of research to back their efficacy, and experts are now calling for tighter guidelines, including a waiting period.”
Imagine the uproar from spine surgeons in the US if a similar moratorium were imposed. Just as we witnessed with the assassination of AHCPR guideline #14, heads would roll on Capitol Hill if any restrictions were placed on spine surgeons.
This threat includes Dr. Tom Price, orthopedist, now in charge at HHS; if he were to follow the ACP and JAMA guidelines promoting DCs as the front-line providers, his colleagues would be livid.
Research and evidence-based practices are fine until they cut into profits, just as we witnessed with the AHCPR guideline.
If you didn’t already know, spine/orthopedic surgeons are the wealthiest MDs who refuse to admit they have perpetrated an inordinate increase in unnecessary spine surgeries that have left a trail of disability, addiction, and hopelessness for millions of failed back surgery victims.
Can we fire spine surgeons who knowingly mislead patients into spine fusions without recommending nondrug care first or a waiting period?
Like their pain management colleagues dispensing opioids like candy and performing ineffective ESI, the aftermath of addiction and disability is just a part of doing business.
And the mere thought of reducing the number of spine surgeries will make every spine surgeon more than “mildly nauseous” – it will make them “bigly” sick to their stomachs.
There is no way they want their cash cow to disappear despite the growing consensus that spine surgeries are too many, too costly, and too ineffective.
Instead, the medical attitude seems to be So What? about the new guidelines or new research criticizing the rise of opioid addictions and needless spine surgery. They have seen other guidelines come and go unable to slow down their medical gravy train.
We’ve also seen no remorse, we’ve heard no contrition, and they offer no mea culpa, but there is plenty of motivation for them to continue on the same fast track since low back pain now amounts to a $177 billion industry.[15]
As Richard Deyo, MD, MPH, wrote, “More people are interested in getting on the gravy train than on stopping the gravy train”[16] and little do people know they’re being taken for a dangerous ride on this medical gravy train until it wrecks.
Taking It Personally
Unless you’ve worked with these failed back surgery patients or know those strung out on opioids or those families decimated with death or addiction, sometimes it’s easy to forget the need to derail this medical gravy train before it wrecks more lives.
If a paradigm shift in spine care is to occur, the public and press need convincing evidence to overcome the bias they’ve learned against chiropractors. With the abundance of evidence I’ve cited in this one paper, a case can easily be made that medical spine care is a bust.
Mark Schoene, associate editor of THEBACKLETTER, a leading international spine research journal states that “such an important area of medicine has fallen to this level of dysfunction should be a national scandal.”[17] Chiropractors more than most understand the size of this scandal is bigger than the public suspects.
Considering the century old “backstory” defaming chiropractors, it will take more than scientific facts and figures to overcome chirophobia to reach a tipping point — it may need an emotional push.
For example, #BlackLivesMatter gained a push when Michael Brown, a black 18-year-old, was shot and killed by a white police officer in Ferguson, Mo.
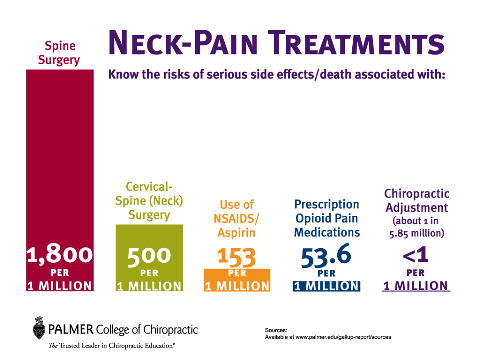
Perhaps we need to highlight a few causalities in the medical war to bring attention to our struggle, #ChiropractorsMatter, which shouldn’t be a problem considering approximately 2500 patients per one million suffer death or severe adverse reactions to medical spine care annually. This figure doesn’t include the 75% of fusion patients who fail to return to work within two years.[18]
Sometimes it has to hit you personally before you understand the gravity of this medical scam in spine care. Just as some white people cannot empathize with #BlackLivesMatter, perhaps people who have not suffered with chronic pain, drugs, and surgery cannot understand how #ChiropractorsMatter.
For example, recently I spoke with a childhood friend of mine about our 50th high school reunion that I missed because I now live 3,000 miles from SoCal. He informed me of the people and events at the reunion, and then parenthetically told me he was going to have minimally-invasive surgery on his SIJ, a chronic problem after felling a tree decades ago. He was not in acute pain nor impaired from working; he just had a persistent pain in the butt.
When he told me he was having surgery, I was stunned.
“John, you do know who you’re talking to, don’t you?”
In fact, he was clueless of my work so I gave him my 5-minute TED Talk about the guidelines that call for 2 to 4 weeks of nondrug, conservative care before any talk about drugs, shots, or surgery. Among other studies, I also mentioned the study[19] finding 75% of fusions fail to return injured workers back to work within two years and most patients get strung out on opioids afterwards.
However, nothing seemed to persuade him to reconsider surgery.
“But my doctor says it’s minimally-invasive.”
We’ve all seen the sales pitch on TV ads from the Laser Spine Institute showing people after surgery with a “one inch band-aides” on their back while frolicking with their dogs and friends.
I explained to John that MIS still cuts to implant screws. Plus, MIS has an extraordinarily high re-operation rate of 38% of patients who required open disc surgery after laser decompression failed to relieve their symptoms.[20]
So it’s not as simple and safe as the TV ads pretend, but it didn’t register with John. Apparently he was convinced to a quick-fix to his back pain no matter what I said.
“But my doctor says…” he kept repeating to every point I made.
To make my sad story short, John had the surgery and then stroked out in recovery; hemiparesis with a blind left eye. A week later John died of “complications from surgery.”
In fact, John died from being misled by his surgeon.
John was a victim of clinical iatrogenesis as well as cultural iatrogenesis—a combination of bad medical advice that refused to follow the guidelines and a culture of contempt for chiropractors nurtured by the AMA propaganda.
I still believe his death would not have happened if he had followed my advice to see a DC first, but chirophobia from a lifetime of medical defamation, misleading ads touting the wonders of minimally invasive surgery, and a greedy surgeon was too much for John to overcome.
He simply didn’t have the “backstory” to understand the context of the controversies about the spine surgery fiasco as I tried to explain to him in my quick chiro TED Talk. Instead, he swallowed the bait, hook, line, and sinker, just as millions of people do every year.
I wonder if John’s surgeon felt “mildly nauseous” after his death.
[1] FBI director says he feels ‘mildly nauseous’ about possibility he affected election, but has no regrets
[2] U.S. Spine Care System in a State of Continuing Decline?, The BackLetter, vol. 28, #10, 2012, pp.1
[3] Centers for Disease Control and Prevention Press Release, CDC Vital Signs: Overdose of Prescription OPR—United States, 1999-2008; 2011: www.cdc.gov/media/releases/2011/t1101_presecription_pain_relievers.html.
[4] Assessing Benefits And Harms Of Opioid Therapy, CDC,
http://www.cdc.gov/drugoverdose/pdf/assessing_benefits_harms_of_opioid_therapy-a.pdf
[5] Centers for Disease Control and Prevention Press Release, CDC Vital Signs: Overdose of Presription Opioid Pain Relievers—United States, 1999-2008; 2011: www.cdc.gov/media/releases/2011/t1101_presecription_pain_relievers.html.
[6] American Public Health Association, “Prevention and Intervention Strategies to Decrease Misuse of Prescription Pain Medication”
[7] Dylan Scott, “1 in 3 Americans blame doctors for national opioid epidemic, ATAT-Harvard poll finds.” Boston Globe, March 17, 2016
[8] Denise Boudreau, PhD, Michael Von Korff, ScD, Carolyn M. Rutter, PhD, Kathleen Saunders, G. Thomas Ray, Mark D. Sullivan, MD, PhD, Cynthia Campbell, PhD, Joseph O. Merrill, MD, MPH, Michael J. Silverberg, PhD, MPH, Caleb Banta-Green, and Constance Weisner, DrPH, MSW. “Trends in De-facto Long-term Opioid Therapy for Chronic Non-Cancer Pain,” Pharmacoepidemiol Drug Saf. 2009 December; 18(12): 1166–1175. doi:10.1002/pds.1833.
[9] Dynamic Chiropractic – May 1, 2017, Vol. 35, Issue 05
[10] Deyo, RA. Low -back pain, Scientific American, pp. 49-53, August 1998.
[11] S Boden, et al. “Emerging Techniques For Treatment Of Degenerative Lumbar Disc Disease,” Spine 28 (2003):524-525.
[12] Murphy DR, Hurwitz EL, Gregory AA, Clary R. A non-surgical approach to the management of lumbar
spinal stenosis: a prospective observational cohort study. BMC Musculoskelet Disord. 2006;7:16.
[13] Private communication with JC Smith, 7/10/2013
[14] John Panagopoulos, BAppSci. (Physiotherapy), BMedSci; Julia Hush, PhD; Daniel Steffens, PhD; Mark J. Hancock, PhD. Do MRI Findings Change Over a Period of up to 1 Year in Patients With Low Back Pain and/or Sciatica? Spine. 2017;42(7):504-512
[15] http://www.beckersspine.com/spine/item/36076-us-spends-789b-yearly-on-neurological-diseases-chronic-low-back-pain-accounts-for-177b.html
[16] Reed Abelson, Financial Ties Are Cited as Issue in Spine Study, NY Times, January 30, 2008
[17] U.S. Spine Care System in a State of Continuing Decline?, The BackLetter, vol. 28, #10, 2012, pp.1
[18] Anderson, Joshua T. BS; Haas, Arnold R. BS, BA; Percy, Rick PhD; Woods, Stephen T. MD; Ahn, Uri M. MD; Ahn, Nicholas U. MD, Single-Level Lumbar Fusion for Degenerative Disc Disease Is Associated With Worse Outcomes Compared With Fusion for Spondylolisthesis in a Workers’ Compensation Setting, Spine: 01 March 2015 – Volume 40 – Issue 5 – p 323–331
[19] Anderson, Joshua T. BS; Haas, Arnold R. BS, BA; Percy, Rick PhD; Woods, Stephen T. MD; Ahn, Uri M. MD; Ahn, Nicholas U. MD, Single-Level Lumbar Fusion for Degenerative Disc Disease Is Associated With Worse Outcomes Compared With Fusion for Spondylolisthesis in a Workers’ Compensation Setting, Spine: 01 March 2015 – Volume 40 – Issue 5 – p 323–331
[20] Brouwer PA et al. Percutaneous laster disc decompression (PLDD) versus conventional microdiscectomy in sciatica: A randomized controlled trial, The Spine Journal, 2015.