“A comprehensive guide to the new science of treating lower back pain”
A review of 80-plus studies upends the conventional wisdom.
Vox Media, Aug 4, 2017
TO: Julia Belluz
RE: Response to your article, “A comprehensive guide to the new science of treating lower back pain”
FROM: JC Smith, MA, DC
Dear Julia,
Let me congratulate you on your well-intentioned essay on the back pain pandemic, a huge problem that has significantly contributed to the opioid crisis and failed back surgery syndrome Americans now experience at catastrophic levels. Please allow me to push-back on some of your assertions as a matter of journalistic fair doctrine.
First of all, there is actually no “new science of treating low back pain” as your title suggests, but rather an effort to incorporate the credible science that currently exists that has been ignored by the medical powers-to-be.
Full disclosure: I speak from clinical experience as a 40-year career chiropractor who specializes in low back pain (LBP), as an author of two books and hundreds of articles on the controversies in spine care, and as director of the website Chiropractors for Fair Journalism.
Since your goal is to help the public understand this issue, let me share with you some of the research that may help you in future articles.
The recent guidelines on low back pain from the American College of Physicians, JAMA, CDC, to name a few, were not from revelations of any “new science of treating low back pain” as you suggest. For example, the 2017 ACP guideline is not really new, just updated from the 2007 version when the American College of Physicians/American Back Pain Society “Guidelines on the Diagnosis and Treatment of Back Pain” also endorsed spinal manipulation, acupuncture, massage therapy, and other CAM treatments for low back pain.[1]
You were correct, however, when you wrote, “A review of 80-plus studies upends the conventional wisdom.” Perhaps this statement might have said “conventional medical wisdom” since drugs, shots and surgeries have been proven ineffective for the vast majority of nonspecific low back pain cases as you noted with your comment, “Despite the clear risks, doctors have continued to prescribe painkillers, and perform surgeries and injections,” which should have been stronger considering the damage these treatments have done.
Mark Schoene, editor of The BackLetter, an international spine journal for healthcare professionals published by Lippincott Williams & Wilkins, agrees medical spine care as a whole is a “national scandal”:
“Medical spine care is the poster child of inefficient care…such an important area of medicine has fallen to this level of dysfunction should be a national scandal. In fact, this situation is bringing the United States disrespect internationally.”[2]
Unfortunately, it took a national opioid crisis causing millions of addictions, hundreds of thousands of deaths, as well as millions of disabled people from chronic low back pain and failed back surgeries to make officials revisit the troubling consequences of medical care for acute and chronic back pain.
These are issues chiropractors have warned the public about for years but were ignored by both the medical profession indifferent to “best practices” evidence and a drug industry hell-bent profiting from drug sales and, unfortunately, a biased media unable to objectively report the benefits of chiropractic and other conservative care treatments.
Hopefully with the new guidelines, this medical charade in spine care will stop, but not without the help of progressive newsmen willing to think out of the medical box to expose this mess as you’ve attempted.
The Elephant in the News Room
I noticed Vox Media’s masthead prides itself on in-depth reporting:
“Go Deeper: Vox Media is a prestigious media company that believes in the power of going deeper to connect with global, passionate, curious audiences.”
I wonder when someone among the thousands of investigative journalists in America and at Vox someone would have asked the obvious question: since back pain is the main cause for the use of opioid painkillers for non-cancerous chronic pain patients, why hasn’t the chiropractic profession been recognized to help solve this problem considering chiropractors offer a nondrug solution that research has shown for years to be more effective than drugs, shots or surgery?
 Indeed, this is the elephant in the newsroom that journalists ignore and an issue that needs to be vetted before this back pain pandemic will improve by changing the public’s awareness.
Indeed, this is the elephant in the newsroom that journalists ignore and an issue that needs to be vetted before this back pain pandemic will improve by changing the public’s awareness.
If just one newsman had opened this can of worms, he or she would have learned this back pain pandemic did not happen by chance but began years ago as the result of an illegal medical boycott that conspired with the media to misinform to the public for decades about chiropractic care in order to corner the lucrative spine care market. At trial it was discovered even the famed columnist Ann Landers was involved by meeting regularly with AMA officials to defame chiropractors in her syndicated columns.
Another obvious question you might consider is why the medical profession still refuses to accept the new guidelines. For example, after the short-lived ballyhoo in the media when the new guidelines were released earlier this year, nothing actually changed. People are still prescribed drugs, shots and surgery, and MDs still refuse to refer to chiropractors.
I really hate to be cynical, but there is simply too much money and too few ethics to do the right thing by referring these pain patients to nondrug practitioners as the guidelines recommend.
Fake News
I must say your bias against chiropractors also came through very clearly both in your text as well as in your choice of experts to describe my profession, namely Cathryn Jakobson Ramin.
Julia, if you wanted a “comprehensive guide to the new science of treating low back pain,” you should have read my book, The Medical War Against Chiropractic—the untold story from persecution to vindication, to gain an in-depth, fair and balanced perspective rather than a distortion of the chiropractic profession.
Instead, you chose to follow the advice of a very questionable source, Cathryn Jakobson Ramin, whose book, Crooked, revealed her jaded opinion of chiropractic rather than a definitive study on the role of chiropractic in the back pain pandemic as the new guidelines suggest.
After reading her book, in no way should she be giving advice to anyone. Ms. Ramin’s chapter on chiropractic care was clearly a hatchet job and a mockery of good journalism—she has proven herself to be an embarrassment to investigative journalists who pride themselves on objective reporting as I revealed in my review of her book, Poisoned Pen.
Julia, some of your own comments were perhaps less helpful than intended, such as:
- “Most recently, in February, 2017, the American College of Physicians advised doctors and patients try ‘non-drug therapies’ such as exercise, acupuncture, tai chi, yoga, and even chiropractics…”
- Incredulously, Julia, your choice of words, “even chiropractics,” exemplifies your own disbelief.
- For your information, chiropractic is not used in the plural—it is simply “chiropractic,” not “chiropractics.”
- You also wrote, “The [Rubinstein] Cochrane review on acute pain found that spinal manipulation worked no better than placebo. So people with a short episode of back pain should probably not bother seeing a chiropractor.”
- This statement is incorrect. In 1994 the most comprehensive “best practices” guideline by an expert panel at the Agency for Health Care & Policy listed manipulation as a “proven treatment” on acute low back pain in adults.
- Roger Chou, MD, renowned researcher, wrote both the 2007 and the updated 2017 versions of the Joint Clinical Practice Guideline for the Diagnosis and Treatment of Low Back Pain for the American College of Physicians and the American Pain Society that also recommended spinal manipulation for both acute and chronic LBP.
- In fact, the Rubinstein review was considered an outlier, not a game-changer, since his study contradicted many other systematic reviews including the ACP review by Chou.
- Here are examples of some systematic reviews that support chiropractic care:
- Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline, by Chou R
- Chiropractic management of low back disorders: report from a consensus process by Globe GA
- Literature syntheses for the Council on Chiropractic Guidelines and Practice Parameters: methodology, by Triano JJ
- Chiropractic management of fibromyalgia syndrome: a systematic review of the literature, by Schneider M
- Chiropractic management of low back pain and low back-related leg complaints: a literature synthesis, by Lawrence DJ
These are just a few of the international systematic reviews casting chiropractic in favorable light rather than the lone review you chose. I also must object to his advice about imaging:
- “As a chiropractor himself, he [Rubinstein] had some advice for patients: They should avoid chiropractors who routinely make X-rays or do advanced diagnostics for low back pain because this adds nothing to the clinical picture, particularly in the case of nonspecific low back pain.”
- I would argue any chiropractor who does not take x-rays should be avoided just as you would avoid a dentist who drills without the benefit of x-rays—in effect, a poke in the dark.
- “Spinal manipulation, the cranking and tweaking on offer [sic] when you visit a traditional chiropractor, is among the most popular approaches to back pain.”
- Julia, at least you’re willing to admit chiropractic is among the most popular treatments, but we chiropractors do no “cranking or tweaking,” nor do we “crack” or “yank” as much as we gently adjust the spinal joints with skillful precision to restore joint play—the prerequisite for a healthy spine. Again, your choice of words appears to demean our art and could, in effect, frighten people to not use our services. Indeed, would you go to a practitioner who “cranked” your spine? I seriously doubt I would.
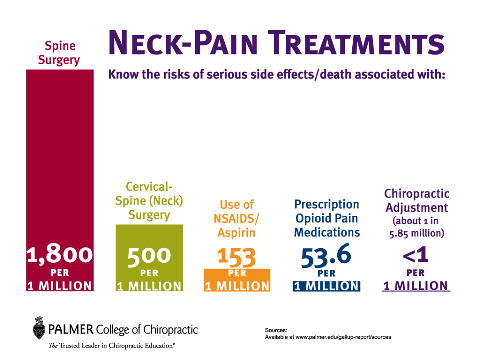
- “While the risks of serious side effects from spinal manipulation for back pain are rare — about one in 10 million — the risks associated with chiropractic therapy for neck pain tend to be slightly higher: 1.46 strokes for every million neck adjustments.”
- Once again, Julia, you failed to mention research that debunks the allegation of manipulation causing stroke, such as the Systematic Review and Meta-analysis of Chiropractic Care and Cervical Artery Dissection: No Evidence for Causation, written by a team of neurosurgeons at the University of Pennsylvania Hershey Medical Center published in February, 2016, that concluded “There is no convincing evidence to support a causal link between chiropractic manipulation and cervical artery dissection (CAD).”
-
- You also missed noting another famous study on stroke and chiropractic care: The Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders: Executive Summary by Scott Haldeman and David J Cassidy, et al. that came to two conclusions:
- There was no smoking gun between cervical manipulation and catastrophic bleeds.
- This study also found a similar association of strokes among patients receiving general practitioner services.
- You also missed noting another famous study on stroke and chiropractic care: The Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders: Executive Summary by Scott Haldeman and David J Cassidy, et al. that came to two conclusions:
In fact, the rate of adverse events associated with chiropractic care is less than having a stroke while in a hair salon or a dentist’s chair,[3] or being hit by lightning (one in 600,000).[4] You also made no mention the rate of death and serious side effects from medical spine care (drugs, surgery) are approximately 2,500 in one million.
Let’s be honest, Julia, who’s hurting who?
Medical Fait Accompli
I expected Vox as “a prestigious media company” to be above such specious journalism, but just as racism is embedded in our society, so is chirophobia—the bias against chiropractors—by misrepresenting the research, ignoring the new guidelines, and insulting our profession with spurious remarks, which was the same goal of the AMA’s Committee on Quackery that referred to DCs as “rabid dogs” and “killers” in its goal to “contain and eliminate” chiropractors.
At the Wilk v. AMA antitrust trial, Judge Susan Getzendanner wrote in her court decision about the damage done to chiropractors’ reputations:
“The activities of the AMA undoubtedly have injured the reputation of chiropractors generally… In my judgment, this injury continues to the present time and likely continues to adversely affect the plaintiffs. The AMA has never made any attempt to publicly repair the damage the boycott did to chiropractors’ reputations.”[5]
Even after this federal court found the AMA guilty of illegal antitrust tactics in its war against chiropractors, little credit was ever given to those chiropractors who stood fast to maintain the art of spinal manipulation.
The American public and press fail to understand in the first half of the 20th century 12,000+ chiropractors were arrested over 15,000 times and 3,300 were sent to prison for the crime of helping sick people get well without the use of drugs, shots or surgery.
If it weren’t for the persistence by thousands of practicing chiropractors, millions more in the public today would be addicted to opioid painkillers and disabled by ineffective back surgeries, yet where is credit given by the media to these chiropractors who endured imprisonment, social ridicule, and economic boycott to carry the flag of drugless care?
Despite its loss in federal court, the AMA was unfazed by this court decision since it had already accomplished its goals to 1) defame its major competition and 2) corner the spine care market. Indeed, the medical war against chiropractors was fait accompli despite the court’s ruling; the damage was done and now it’s impossible to put the toothpaste back in the tube.
Perhaps it’s time for people in the media to give chiropractors a pat on their backs for surviving the medical war to bring a safe and effective nondrug, nonsurgical treatment to a world suffering with chronic pain that is now heralded among the top treatments as Anthony Rosner, PhD, testified before The Institute of Medicine:
“Today, we can argue that chiropractic care, at least for back pain, appears to have vaulted from last to first place as a treatment option.”[6]
Chiropractic Clarification
Let me help you dig deeper into the back pain equation about the role chiropractic care plays to help rather than hinder the public’s understanding of this massive problem.
In your previous article on Feb. 14, 2017, Doctors finally admit drugs can’t fix most cases of back pain, you spoke there is “no detectable cause” about nonspecific low back pain. Your comment warrants an explanation if you want to clarify rather than confuse your readers:
Doctors talk about back pain in a few different ways, but the kind most people suffer from is what they call “nonspecific low back pain.” To be clear, this kind of low back pain has no detectable cause — like a tumor, pinched nerves, osteoporosis, or a fracture.
To the contrary, Julia, there are very good explanations for the causes of non-specific LBP, but this requires thinking out of the medical box of “red flag” causes as you suggest – “like a tumor, pinched nerves, osteoporosis, or a fracture.” I might add to your list, “bad discs,” the leading misdiagnosis given for LBP cases.
Instead, the chiropractic literature speaks in terms of biomechanical issues such as joint play, joint dysfunction, vertebral subluxation complex, spinal compression, manipulable lesion, joint complex dysfunction, and segmental buckling that comprise the majority of these non-specific conditions.
Aside from the 23 discs in the spinal column that physicians focus on to sell “bad disc” surgeries to gullible patients, the most overlooked yet obvious aspect of spinal anatomy is the fact the spine is a dynamic yet precarious weight-bearing pillar of interconnecting 24 vertebrae with hundreds of joints – the missing link in the public’s concept of back pain.
Counting all the vertebral joints, sacroiliac joints, rib heads, and pelvis, research now suggests the total number of joints is 364, a fact lost to most physicians and the public. This total includes all synovial, symphysis, and syndesmosis joints in the spine, according to Gregory D. Cramer, DC, PhD, Dean of Research at National University of Health Sciences.[7]
It has been my experience most people don’t realize the spine has any joints because all they hear from their MDs are “pulled muscles” and “bad discs.”
The anatomy and physiology of the spine suggests spinal joint function (a concept called “joint play”) is more important than how discs look on an image. In fact, discs are merely cartilaginous shock absorbers secondary to the spinal biomechanics and do nothing until the spine’s normal motion becomes altered due to trauma (usually starting with childhood accidents, sport injuries, lifting with bad leverage) that is later exacerbated by some type of passive compressive force such as prolonged sitting.
In light of spinal biomechanics, you can see how the medical diagnosis of “bad discs” is both simplistic and does not address the primary cause of altered spinal biomechanics in these nonspecific back pain cases.
The tsunami of spine fusions based on a debunked ‘bad disc’ theory has been chided as irrelevant as “finding grey hair” and dubbed “incidentalomas” since they also occur in pain-free people.[8]
The Mayo Clinic did a systematic review of “bad discs” and concluded they are ubiquitous as part of the aging process. As you can see on Table 2, 80% of asymptomatic patients by age 50 will show signs of disc degeneration, but they have no pain.
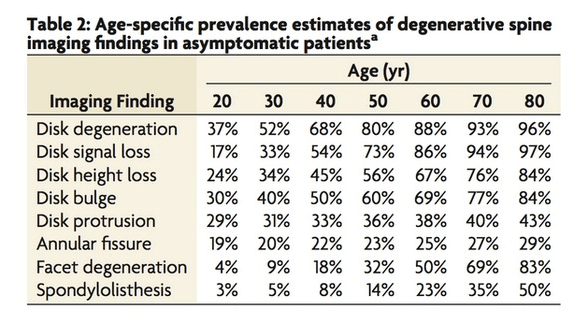
Obviously the debunked “bad disc” diagnosis is not the underlying cause of most back pain, yet few surgeons reveal this truth to patients, instead telling them fusion is the answer to their “bad disc.”
John McMillan Mennell, MD, who testified at the Wilk v. AMA antitrust trial, was a distinguished orthopedist, professor at eight medical schools, and expert on manipulative therapy. He mentioned the value of spinal manipulative therapy (SMT), the backbone of chiropractic care:
“Manipulative therapy relieves symptoms of pain arising from mechanical joint dysfunction and restores lost joint function. No other modality or physical treatment can do this as effectively… If you don’t manipulate to relieve the symptoms from this condition of joint dysfunction, then you are depriving the patient of the one thing that is likely to relieve them of their suffering.” I would suspect that nearly 20 million Americans today could be spared suffering and be returned to normal pain-free life were manipulation therapy as readily available to them as empirical nonspecific drug treatment is.”[9]
With the biomechanical concept of joint dysfunction in mind, you can better understand why any treatment that restores proper joint motion helps patients, such as chiropractic adjustments, flexibility and strengthening spinal exercises, yoga, massage therapy, inversion tables, etc.
On the other hand, nothing done by the MD restores joint play, whether it is drugs, shots or disc fusions that actually decrease joint play. In fact, surgery permanently fuses the spine in a misaligned position, which explains the 75% failure rate for lumbar fusion that leads to chronic opioid use.
Indeed, many of these medical interventions are now deemed placebo, facts the public has yet to learn:
o On May 4, 2017, a VA study was released, “Strategies for Prescribing Analgesics Comparative Effectiveness (SPACE).” Erin E. Krebs, MD, MPH, and colleagues from the Minneapolis Veterans Health Care System, found “Opioids are perceived as strong pain relievers, but our data showed no benefits of opioid therapy over non-opioid medication therapy for pain.” In other words, Hydrocodone is no more effective than Motrin.
- In 2015, a major review by Roger Chou, MD, et al. sponsored by the U.S. Agency for Healthcare Research and Quality (AHRQ) found the evidence in favor of spinal injections to be distinctly “underwhelming.”[10]
- Australian spine surgeon Ian Harris suggested spine surgery was “the ultimate placebo” in his book, Surgery, the Ultimate Placebo: A Surgeon Cuts through the Evidence. According to Dr. Harris, spine fusion is not only ineffective but often leads to complications and even when it appears to work it’s usually because of the placebo effect.
MDs Untrained, Dangerous
Another elephant in the newsroom is the fact most MDs are incompetent both in training and treatments. Numerous studies show MDs are very poorly trained on musculoskeletal disorders, which is a huge problem in this pandemic of back pain since the majority of patients seeks MDs initially.
The education inadequacy of MDs was revealed in a study, “Improved education in musculoskeletal conditions is necessary for all doctors,” by Kristina Åkesson, et al:
“Surveys show that undergraduate medical students spend very few hours on the musculoskeletal system, both in basic science and in clinical training. It would be considered negligent for a medical graduate to be incompetent at adequately assessing the heart or lungs, yet it is quite common for students to leave medical school without being able to make a general assessment of the musculoskeletal system.”
Dr. Marc Siegel at FOX News admitted medical primary care providers have only 9 hours of education on “back” and he blamed the opioid epidemic on his own colleagues and pharmacists. “We’re getting a growing awareness of two things: the abuse of back surgery and the abuse of opioids.”[11]
Click on arrow to begin video.
Most remarkably he was very supportive of chiropractic care and other nondrug therapies as part of an integrative teamwork to solve the pandemic of pain and opioid abuse. If only more MDs thought this way we might not have the present crisis.
Fortunately some do, such as Rick Deyo, MD, MPH, researcher/author, who mentioned chiropractic was an effective solution:
“Chiropractic is the most common choice, and evidence accumulates that spinal manipulation may indeed be an effective short-term pain remedy for patients with recent back problems.” [12]
He also admitted to the “outdated ideas” of medical education:
“Calling a physician a back-pain expert, therefore, is perhaps faint praise—medicine has at best a limited understanding of the condition. In fact, medicines’ reliance on outdated ideas may have actually contributed to the problem.”[13]
Scott Boden, MD, director of the Emory Spine Center, also noted most MDs are inept on musculoskeletal disorders (MSDs):
“Many, if not most, primary care providers have little training in how to manage musculoskeletal disorders.”[14]
The National Pain Strategy also mentioned MDs are ill-prepared to manage this opioid crisis:
“Physicians are not adequately prepared and require greater knowledge and skills to contribute to the cultural transformation in the perception and treatment of people with pain.”[15]
More studies have shown:
- MDs are “inept” in their training on musculoskeletal disorders,[16]
- more likely to ignore recent guidelines,[17]
- most likely to be “promiscuous prescribers”[18] and
- more likely to suggest spine surgery than surgeons themselves,[19]
- and, due to their chirophobia, only 2% of medical PCPs refer to DCs despite our superior training and results.[20]
Perhaps the most shocking study found 70% of osteopathic graduates failed to attain a passing score on the MSD competency examination.[21] For a profession whose roots began in manipulative therapy, osteopaths today have fallen far from their founder’s tree.
The authors of a Johns Hopkins survey concluded, “This discrepancy appears to persist beyond the training years and into the realm of clinical practice.”[22]
Mark Schoene makes the case primary care medical practitioners are actually dangerous to patients:
“One can make the argument that the most perilous setting for the treatment of low back pain in the United States is currently the offices of primary care medical practitioners—primary care MDs. This is simply because of the high rates of opioid prescription in these settings. Low back pain has helped trigger a lethal and growing heroin addiction epidemic in the United States. How could that be? Unfortunately, it is easy to connect the dots.”[23]
Mr. Schoene also balks at the proposal to use MDs as the portal of entry for chronic pain patients considering they created this opioid epidemic with their promiscuous prescribing:
“Primary care physicians and pain specialists don’t have unimpeachable backgrounds in the management of chronic pain in the U.S. These are the medical professions primarily responsible for the opioid overtreatment crisis. Are the two professions that helped create the worst pain management crisis in history of modern medicine capable of leading the way forward? That remains to be seen.”[24]
Certainly local MDs will never admit to their lack of training in musculoskeletal disorders, so patients remain blind to the fact their favorite family medical PCP is most likely badly informed about MSDs while recommending ineffective treatments.[25]
This medical mismanagement can be summarized with this equation: bad training + outdated practices + chirophobia + greed = an epidemic of narcotic addiction and back surgeries.
Trading Places
Julia, undoubtedly if you were to dig deeper into the back pain dilemma, you will discover the logical answer to this back pain crisis is for chiropractors to assume the role as primary spine care providers since MDs have proven inept using dangerous methods.
You may recall the 1983 film Trading Places with Eddie Murphy and Dan Akroyd where a snobbish investor and a wily street con artist find their positions reversed as part of a bet by two callous millionaires.
This is exactly what needs to be done—have chiropractors trade places with MDs as primary spine providers. Fortunately, this paradigm shift is slowly happening due to new comparative studies on clinical and cost-effectiveness.
An analysis by Richard Sarnat, MD, and James Winterstein, DC, shows patients enrolled in the chiropractic network experienced fewer hospital visits, spent less time in the hospital for care, underwent fewer surgeries and used far fewer pharmaceuticals than other HMO patients who received traditional medical care, resulting in low utilization costs and high patient satisfaction scores.
According to Dr. Sarnat:
“The AMI study really shows the enormous power and benefit of two things: 1) the utilization of chiropractic in a primary care setting; and 2) the magnitude of outcomes, both clinical and cost, that can be achieved when all members of the health sciences work together as a team for the betterment of the patient, putting aside all professional rivalries. Hopefully, these results are so dramatic that they will ‘wake up’ the health care system (or lack thereof) to the immediate need for true integration among all qualified health care providers.”
Increasingly chiropractors are now considered the best portal for primary spine care providers as the Optum report concluded:
In 2013, the Optum Health internal analysis of low back pain treatments determined the best track to take for cost efficiency begins with a patient consulting a chiropractor first.[26] When a chiropractor was the first provider, treatments were “well-aligned with clinical evidence; the least fragmentation of care; low rates of imaging, injections, and prescription medications; and low total episode cost when manipulation is introduced within the first 10-days of the episode.”[27]
Due to our superior education in MSDs, our proven nondrug, nonsurgical treatments for LBP, our cost and clinical effectiveness, and our proven safety compared to medical spine care, DCs aptly deserve to be America’s primary spine providers.
If it weren’t for the medical war against chiropractors, our role as primary spine care providers would be a foregone conclusion, just as dentists are primary dental providers.
Power to the People
A recent Gallup-Palmer Chiropractic College report found Americans prefer drug-free pain management. While 22% of U.S. adults prefer to take pain medication prescribed by doctors to treat their physical pain, 78% prefer other ways to address their physical pain before they take pain medication.
The Gallup report also found positive feedback from consumers who have used chiropractic care:
- 95% of chiropractic users say it was effective
- 97% of past users would use it again
- 89% of chiropractic users would refer their family and friends
- 88% of past users agree it is a good value
In other patient surveys, chiropractors have consistently ranked as the top treatment for back pain, including Consumer Reports, the military health services, and Medicare surveys.
- In 2013, Consumer Reports published “The Better Way to Get Back Pain Relief: Growing research suggests that drugs and surgery may not be the answer for your bad back,” in which they surveyed more than 14,000 subscribers who ranked chiropractic care the #1 preferred treatment for low back pain in its survey among readers.[28]
Consumer Reports also published two positive articles soon after the ACP and JAMA guidelines were released:
- Stop Back Pain Without Drugs by Sally Wadyka, Consumer Reports, February 14, 2017.
“For the first time, the American College of Physicians is advising treating back pain with nondrug measures like tai chi, yoga, chiropractic, and massage before resorting to over-the-counter or prescription pain relievers.”
- Spinal Manipulation Can Ease Your Aching Back by Teresa Carr, Consumer Reports, April 11, 2017.
“A new analysis finds that the hands-on technique works as well as pain drugs and is safer, too…When you wrench your back, your first impulse may be to rummage through the medicine cabinet for an over-the-counter pain drug or even ask your doctor to prescribe a strong opioid painkiller such as Percocet or Vicodin. But an analysis published April 11 in the Journal of the American Medical Association finds that spinal manipulation can ease your backache and get you moving again without the risk of medication side effects.”
Recently the RAND Corporation released “Complementary and Alternative Medicine in the Military Health System,” highlighting the use and approval of CAM in the military health services:
- Chiropractic is by far the most frequently utilized service (14,000 estimated visits per month – “nearly double the utilization figures for acupuncture, biofeedback, hypnosis and massage combined.”
- Almost two-thirds of Military Treatment Facilities say chiropractic improves patient satisfaction and patients’ quality of life (65 percent and 63 percent, respectively); 57 percent say it improves functional status; 55 percent say it improves work performance; and 45 percent say it improves sleep.
In a Congressionally-mandated pilot project conducted from April, 2005, to March, 2007, testing the feasibility of expanding chiropractic services in the Medicare program,
- 87 percent of patients in the study gave their chiropractor a level of 8 or higher
- 56 percent rated their chiropractor with a perfect 10. [29]
Keep in mind these benefits were delivered without the use of any drugs, shots or surgery. Our brand of spine care has never caused an opioid crisis of addiction or deaths nor left a wake of disability from failed back surgery.
Even the North American Spine Society released its own guidelines supportive of chiropractic care:
- In 2007, the NASS published Diagnosis and Treatment of Degenerative Lumbar Spinal Stenosis. This study provides Level IV therapeutic data suggesting that distraction manipulation and neural mobilization may be beneficial in the treatment of lumbar spinal stenosis.
- In 2010, the NASS released “Contemporary Concepts in Spine Care: Spinal Manipulation Therapy for Acute Low Back Pain” recommending spinal manipulation—5 to 10 sessions over 2 to 4 weeks—should be considered before surgery.
- In 2012, the NASS also published Clinical Guidelines for Multidisciplinary Spine Care Diagnosis and Treatment of Lumbar Disc Herniation with Radiculopathy that found “patients with lumbar radiculopathy due to lumbar disc herniation, 60% will benefit from spinal manipulation to the same degree as if they undergo surgical intervention. For the 40% that are unsatisfied, surgery provides an excellent outcome.”
Medical Chauvinism
With the new guidelines in place, the question now is will MDs actually follow these new guidelines and refer LBP cases to chiropractors? Indeed, what good are research and “best practices” guidelines if the medical profession refuses to integrate them?
Undoubtedly the new guidelines will be met with the same resistance by MDs as we witnessed in 1994 with the AHCPR Guideline #14 on acute low back pain in adults that should have revolutionized spine care, but was sabotaged by the North American Spine Society (NASS) with former Rep. Newt Gingrich (R-GA) leading the charge on Capitol Hill to kill the agency with their mantra, “We ain’t gonna have no bureaucrats telling us how to practice medicine,” an example of political medicine at its worst.
Mark my word: in a year from now do you expect this medical mess in spine care have changed substantially? If history is any proof, it will not. This medical resistance remains the biggest hurdle in the quest to improve spine care in America. Few understand the political power and wrath of spine surgeons, the most powerful medical society in the country and on Capitol Hill.
Unfortunately, medical chirophobia remains the largest impediment to implementing the new guidelines.
For example, Susan and Henry Samueli announced a $200 million donation to the University of California, Irvine, to launch a new health program dedicated to integrative medicine. Obviously this will help to understand how CAM works as well as make it more available to the public.
As to be expected, medical trolls such as Dr. Steven Novella, the director of Science Based Medicine, a group of alt-right naysayers to alternative care, could not resist bashing this effort despite the new guidelines.
“This is ultimately a very bad thing,” said Novella, a neurologist at Yale University and longtime critic of alternative therapies. “It’s putting emphasis and the imprimatur of a university on things that have been discarded as medical fraud for 50 years.”
Oh, really…”a very bad thing…medical fraud for 50 years…” just where is his proof?
His comment reveals how far from the truth he is considering the new guidelines felt confident to endorse CAM providers who, by the way, actually see more patients annually than MDs according to David Eisenberg, MD, from the Osher Institute at Harvard.[30]
Dr. Eisenberg found in 1990 Americans made more office visits to non-MDs than they did to their medical doctors. In fact, this trend to alternative health care had increased by more than 50% in a seven-year span to the astronomical number of 629 million visits compared to only 386 to MDs.
Upon seeing the huge number of Americans using CAM practitioners, Dr. Eisenberg concluded, “Maybe ‘alternative’ isn’t so alternative anymore.”[31]
We cannot expect any significant change in the management of chronic pain despite the new guidelines because Novella and the AMA have no interest to follow any guideline that takes money out of their pockets. Nor do MDs want to be told how to practice better medicine or, god forbid, refer patients to chiropractors. Medical bigotry remains firmly embedded in their chirophobic DNA along with their “halo effect” of superiority.
However, one forthright physician, Aaron E. Carroll, wrote in the New York Times an insightful analysis, “For Bad Backs, It May Be Time to Rethink Biases About Chiropractors.” Finally, an honest MD willing to admit to his bias about chiropractic care!
“A physician like me might suggest any number of potential treatments and therapies. But one I never considered was a referral for spinal manipulation. It appears I may have been mistaken. For initial treatment of lower back pain, it may be time for me (and other physicians) to rethink our biases.”
His admission is huge; now if we could get the other half million MDs to admit to their bias, let alone get a public apology by the AMA for the years of misleading the public, it would explain to the public and press that the medical war against chiropractors was unwarranted, illegal, and also led to the collateral damage of millions of patients addicted to opioids and suffering from failed back surgery.
Can you imagine, Julia, the millions of back pain patients who have been misdiagnosed, misinformed, and mistreated by MDs and the billions of dollars wasted? Imagine the billions of dollars DCs could reduce the national healthcare budget by substituting safe, effective, and much less expensive alternatives for ineffective and expensive medical spine care if America had free enterprise in healthcare treatments instead of the present medical monopoly.
Lastly, Julia, I apologize for my lengthy response to your article, but I felt compelled to elaborate on this important topic of back pain care by giving you the chiropractic backstory behind this opioid crisis and medical spine care mismanagement, a story you and most of the public have never known.
It’s getting harder to sweep chiropractic care under the newsroom rug as more evidence comes forth and the guidelines now recommend. Hopefully this information will spark you to write another follow-up article that encourages people to seek chiropractors first as the guidelines and experts now suggest.
[1] Chou et al., Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Annals of Internal Med., 2007, vol. 147 no.7
[2] U.S. Spine Care System in a State of Continuing Decline?, the BackLetter, vol. 28, No. 10, 2012, pp.1
[3] Management of Medical Emergencies in the Dental Office: Conditions in Each Country, the Extent of Treatment by the Dentist, Anesth Prog. 2006 Spring; 53(1): 20–24.
[4] Allan G.J. Terrett, Current Concepts in Vertebrobasilar Complications Following Spinal Manipulation (West Des Moines, IA: NCMIC Group Inc., 2001).
[5] Getzendanner, Memorandum Opinion and Order, p. 10
[6] Testimony before The Institute of Medicine: Committee on Use of CAM by the American Public on Feb. 27, 2003.
[7] Cramer, G.; Darby, S. 2014 Clinical anatomy of the spine, spinal cord, and ANS. 3rd Edition, Elsevier/Mosby, St. Louis, 559 illustrations, 672pp. Appendix I, pp. 638-642.
[8] RA Deyo, “Conservative Therapy for Low Back Pain: Distinguishing Useful From Useless Therapy,” JAMA 250 (1983):1057-62
[9] G Null, PhD, “Medical Genocide, Part Four: Painful Treatment,” Penthouse (November 1985).
[10] Major Review Finds Scant Evidence to Support Spinal Injections as Treatments for Back and Leg Pain, BackLetter: June 2015 – Volume 30 – Issue 6 – p 64–65
[11] Dynamic Chiro, May, 2017: http://www.dynamicchiropractic.com/digital/index.php?i=1228&a_id=57942&pn=1&r=t#1
[12] Deyo, RA. Low -back pain., Scientific American, pp. 49-53, August 1998.
[13] Deyo, RA. Low -back pain, Scientific American, pp. 49-53, August 1998.
[14] S Boden, et al. “Emerging Techniques For Treatment Of Degenerative Lumbar Disc Disease,” Spine 28 (2003):524-525.
[15] http://iom.nationalacademies.org/Reports/2011/Relieving-Pain-in-America-A-Blueprint-for-Transforming-Prevention-Care-Education-Research.aspx, pp.5.
[16] EA Joy, S Van Hala, “Musculoskeletal Curricula in Medical Education– Filling In the Missing Pieces, The Physician And Sports Medicine,” 32/11 (November 2004).
[17] PB Bishop et al., “The C.H.I.R.O. (Chiropractic Hospital-Based Interventions Research Outcomes) part I: A Randomized Controlled Trial On The Effectiveness Of Clinical Practice Guidelines In The Medical And Chiropractic Management Of Patients With Acute Mechanical Low Back Pain,” presented at the annual meeting of the North American Spine Society, Austin, Texas, 2007; Spine,
[18] Jonathan Chen, Overprescribing of opioids is not limited to a few bad apples, Stanford Medicine News Center, Dec 14 2015
[19] SS Bederman, NN Mahomed, HJ Kreder, et al. In the Eye of the Beholder: Preferences Of Patients, Family Physicians, And Surgeons For Lumbar Spinal Surgery,” Spine 135/1 (2010):108-115,
[20] Matzkin E, Smith MD, Freccero DC, Richardson AB, Adequacy of education in musculoskeletal medicine. J Bone Joint Surg Am 2005, 87-A:310-314
[21] Stockard AR, Allen TW. Competence levels in musculoskeletal medicine: comparison of osteopathic and allopathic medical graduates. J Am Osteopath Assoc. 2006 Jun;106(6):350-5
[22] Medical Student Musculoskeletal Education, An Institutional Survey, Nathan W. Skelley, MD, Miho J. Tanaka, MD, Logan M. Skelley, BS, and Dawn M. LaPorte, MD, Investigation performed at the Department of Orthopaedic Surgery, The Johns Hopkins University, Baltimore, Maryland
[23] The BackLetter, volume 30, number 10, 2015
[24] Why Should the National Pain Strategy Be MD-Centric? BackLetter: February 2016 – Volume 31 – Issue 2 – p 16
[25] Fowler PJ, Regan WD. The patient with symptomatic chronic anterior cruciate ligament insufficiency. Results of minimal arthroscopic surgery and rehabilitation. Am J Sports Med. 1987 Jul-Aug;15(4):321-5
[26] Thomas M. Kosloff, DC, David Elton, DC, Stephanie A. Shulman, DVM, MPH, Janice L. Clarke, RN, Alexis Skoufalos, EdD, and Amanda Solis, MS, Conservative Spine Care: Opportunities to Improve the Quality and Value of Care, Popul Health Manag. Dec 1, 2013; 16(6): 390–396.
[27] Thomas M. Kosloff, DC, David Elton, DC, Stephanie A. Shulman, DVM, MPH, Janice L. Clarke, RN, Alexis Skoufalos, EdD, and Amanda Solis, MS, Conservative Spine Care: Opportunities to Improve the Quality and Value of Care, Popul Health Manag. Dec 1, 2013; 16(6): 390–396.
[29] WB Stason, G Ritter, DS Shepard, C Tompkins, TC Martin, S Lee, “Report to Congress on the Evaluation of the Demonstration of Coverage of Chiropractic Services Under Medicare,” (June 16, 2009)
[30] DM Eisenberg, RC Kessler, C Foster, FE Norlock, DR Calkins, TL Delbanco, “Unconventional Medicine In The United States–Prevalence, Costs, And Patterns Of Use,” N Engl J Med 328 (1993):246-252.
[31] DM Eisenberg, RC Kessler, C Foster, FE Norlock, DR Calkins, TL Delbanco, “Unconventional Medicine In The United States–Prevalence, Costs, And Patterns Of Use,” N Engl J Med 328 (1993):246-252
