January 20, 2011
TO: Michael W. O’Bar
Deputy Chief
TRICARE Policy and Operations
Office of the Assistant Secretary of Defense
Health Affairs
Skyline Five, Suite 810, 5111 Leesburg Pike
Falls Church, Virginia 22041-3206
Dr. S. Ward Casscells
The Assistant Secretary of Defense
1200 Defense Pentagon
Washington, DC 20301-1200
FROM: JC Smith, MA, DC
1103 Russell Parkway
Warner Robins, GA 31088
RE: Discrimination against Chiropractic Care in TRICARE
Dear Sir:
I read your letter of December 6, 2010 with interest, but was confused by your bottom line that the reason chiropractic care is not available to all military or TRICARE recipients is due to:
“In addition, adding chiropractic care to the primary car model was estimated to increase the number of visits per episode of care. Ultimately, this increases the costs and delays a service member’s return to duty. These constraints have limited our ability to field chiropractic care beyond the 60 locations currently providing the service.”
I was most perplexed by this summation since it ignored the positive data from the two attachments included in your letter: Chiropractic Care Study and the Study Relating to Chiropractic Services and Benefits.
After reviewing your letter and the letter from S. Ward Casscells, MD, I think a case can be made what we see is the continued interference of the medical bureaucracy to obstruct the will of Congress to make chiropractic care accessible to active military and TRICARE recipients. Indeed, the facts simply do not support your conclusion.
Contradictory Conclusions
First of all, a September 22, 2009 letter to Congressmen from Ellen P. Embrey, then Deputy Assistant of Defense, clearly stated: “The [Chiropractic Care Study] report reveals that our Active Duty members are very satisfied with the chiropractic care they receive, and military treatment facility personnel consider offering chiropractic care to be beneficial.”
Somehow your conclusions failed to consider Ms. Embrey’s opinion or the enormously high patient satisfaction rates that ranged from 94.3 percent in the Army; the Air Force tally was also high with twelve of 19 bases scoring 100 percent; the Navy also reported ratings in the 90 percent or higher; even your own TRICARE outpatient satisfaction surveys (TROSS) rated chiropractors at 88.54, which was 10 percent “higher than the overall satisfaction with all providers” that scored at 78.31 percent.[1]
This Chiropractic Care Study also commented on the Unit Commanders and MTF personnel concerning chiropractic care. “The responses were overwhelmingly a five (the highest rating available); MTFs that offer chiropractic care are pleased to do so.”
This survey also contradicts one of your claims that chiropractic care “delays a service member’s return to duty.” According to this survey, when asked “do you think chiropractic care returns Active Duty Service Members (ADSM) to duty faster?” the study concluded “Once again, it was generally positive.”[2]
Another question posed to the ADSM was the likelihood to select chiropractors over osteopaths or physical therapists (five being very likely), the response was again very positive with “responses from threes to fives.”[3]
“Overall, the surveys showed that MTFs consider chiropractic care a valuable adjunct to the care offered in the MTFs. Unit personnel generally consider chiropractors to return ADSMs to duty faster, and they would select a chiropractor as much or more than a Doctor of Osteopathy or physical therapist.”[4]
Considering the results of your own survey, it is bewildering how your report came to its conclusion unless there was some bias or tampering. Certainly the reasoning to limit chiropractic care flies in the face of this Chiropractic Care Study. Both ADSM and Unit Personnel are very pleased with chiropractic care, “generally consider chiropractors to return ADSMs to duty faster,” and most prefer chiropractic care over osteopaths or PTs.
This report also ignored another important study: as far back as 1972, a scientific study of more than six hundred employees entitled “Industrial Back Injury” by C. Richard Wolf, MD, found chiropractic care had a 2:1 superiority over traditional medical care for low back cases.[5]
The study covered light to major injuries (some with more than 60 days of lost time) and concluded:
- Employee statement of lost time; 32 days average for MD-treated group versus 15.6 days average for the chiropractor-treated group.
- Percentage of employees reporting lost time in excess of 60 days, 13.2 percent of those treated by MDs versus 6.7 percent of those treated by doctors of chiropractic; and
- Percent of employees reporting no lost time, 21 percent of those treated by MDs versus 47 percent of those treated by doctors of chiropractic.
Several other states such as Oregon, Kansas, Iowa, Montana, and Wisconsin have compiled similar data showing chiropractic was superior to medical care for industrial back injuries. Every study showed chiropractic care reduced work days lost, treatment length, and treatment costs, all points ignored by Dr. Casscells.
Ignoring these positive outcomes by TRICARE is reminiscent of the battle when chiropractors sought Medicare coverage. Recall this battle came during the intense medical war against chiropractic in the 1960s when the AMA’s Committee on Quackery was in full force with propaganda and tampering with Congressmen. The COQ advised its medical members on the HEW Sec. Cohen’s Medicare panels to focus criticism on chiropractic’s allegedly “dangerous,” “poorly educated,” and “unscientific” basis. Of course, these allegations were proven untrue despite the best efforts of the AMA’s propaganda to promote this nonsense.
Instead of these previous medical allegations, Dr. Casscells now uses new but also unproven allegations: “increases the costs and delays a service member’s return to duty.” The delay in return to duty conflicted with the active duty personnel’s own comments, and the increase in cost also failed to consider the substitution of chiropractic care for medical services. Imagine the huge savings when chiropractic care can avoid back surgery. To omit this substitution effect is a huge oversight by Dr. Casscells.
The second report you sent to me concerning chiropractic care, “Report to Congress, Study Relating to Chiropractic Services and Benefits, Section 712, National Defense Authorization Act for FY07,” also revealed peculiar conclusions made by Dr. Casscells, MD, the Assistant Secretary of Defense, Health Affairs.
In his letter of March 3, 2009, Dr. Casscells jumped to a few unsupported conclusions:
- “Despite some evidence for superiority of spinal manipulation therapy over no treatment of placebo treatment, the reports found no evidence for clear benefits in comparison to other commonly used treatments for nonspecific low back pain or nonspecific neck pain.”[6]
Apparently Dr. Casscells did not look very hard to find studies that support chiropractic care. His erroneous conclusion flies in the face of recent research. In an article, “Are There Any Effective Nonsurgical Treatments for Painful Disc Herniations?” Jo Jordan, PhD, wrote that spinal manipulation may be “The lone ray of light among nonsurgical treatments in this review concerned spinal manipulation.” [7]
According to the 1993 Manga Report , “The Effectiveness and Cost-Effectiveness of Chiropractic Management of Low-Back Pain,”[8] this evidence-based study concluded spinal manipulation was the “therapy of choice for most low back pain”:
In our view, the constellation of the evidence shows:
- The effectiveness and cost-effectiveness of chiropractic management of low-back pain.
- The untested, questionable or harmful nature of many current medical therapies.
- The economic efficiency of chiropractic care for low-back pain compared with medical care.
- The safety of chiropractic care.
- The higher satisfaction levels expressed by patients of chiropractors.
The following is a review of the numerous international and American guidelines that recommend spinal manipulation for both acute and chronic low back pain:
- 1978: New Zealand Royal Commission on Chiropractic
- 1990: RAND study on appropriateness of spinal manipulation
- 1990: Meade Study (UK) comparing manipulation vs. hospital care
- 1993: Manga Report Ontario (Canada) Ministry of Health
- 1994: AHCPR Acute Low Back Pain Guideline
- 1994: Clinical Standards Advisory Group (UK)
- 1995: Council on Chiropractic Guidelines and Practice Parameters
- 2003: Ontario Workers’ Safety and Insurance Board
- 2003: Norway Spine Study
- 2004: European Back Pain Guidelines.
- 2004: The UK Back Pain Exercise And Manipulation (UK BEAM) Trial
- 2004: Swedish Lumbar Spine Study
- 2007: Guideline on Back Pain: American College of Physicians
- 2008: Decade of Bone & Joint Disorders: CLBP
- 2008: The Bone and Joint Decade Task Force on Neck Pain and Its Associated Disorders
- 2009: The National Institute for Clinical Excellence (UK-NICE)
As well, an editorial in the Annals of Internal Medicine published jointly by the American College of Physicians and the American Society of Internal Medicine (1998) noted that” spinal manipulation is the treatment of choice”:
The Agency for Health Care Policy and Research (AHCPR) recently made history when it concluded that spinal manipulative therapy is the most effective and cost-effective treatment for acute low back pain[9]. The 1994 guidelines for acute low back pain developed by AHCPR concluded that spinal manipulation hastens recovery from acute low back pain and recommended that this therapy be used in combination with or as an alternative to non-steroidal anti-inflammatory drugs. At the same time, AHCPR concluded that various traditional methods, such as bed rest, traction, and other physical and pharmaceutical therapies were less effective than spinal manipulation and cautioned against lumbar surgery except in the most severe cases.
Perhaps most significantly, the guidelines state that unlike nonsurgical interventions, spinal manipulation offers both pain relief and functional improvement. One might conclude that for acute low back pain not caused by fracture, tumor, infection, or the cauda equina syndrome, spinal manipulation is the treatment of choice. [10] (emphasis added)
Many ethical medical physicians now speak out in favor of chiropractic care. William Lauerman, MD, chief of spine surgery, professor of orthopedic surgery at Georgetown University Hospital states: “I’m an orthopedic spine surgeon, so I treat all sorts of back problems, and I’m a big believer in chiropractic.”[11]
Richard Deyo, MD, MPH, mentioned chiropractic as a solution: “Chiropractic is the most common choice, and evidence accumulates that spinal manipulation may indeed be an effective short-term pain remedy for patients with recent back problems.”[12]
Gordon Waddell, MD, also suggested chiropractic care as a solution: “There is now considerable evidence that manipulation can be an effective method of providing symptomatic relief for some patients with acute low back pain.”[13]
Dr. Casscells’ concluded that “the implementation of chiropractic services and benefits would not be feasible given the budgetary requirements and the findings relative to medical readiness.” Once again his conclusion belies the facts.
His belief that chiropractic care would “not be feasible given the budgetary requirements” contradicts the finds of a comparative study on back pain published in the Archives of Internal Medicine in 2004 that shows chiropractic care is the best buy. This study ascertains the effect of systematic access to chiropractic care within a large managed-care system that showed chiropractic care to be both “clinically beneficial” and “may reduce overall health care costs”:
Conclusions: Access to managed chiropractic care may reduce overall health care expenditures through several effects, including (1) positive risk selection; (2) substitution of chiropractic for traditional medical care, particularly for spine conditions; (3) more conservative, less invasive treatment profiles; and (4) lower health service costs associated with managed chiropractic care. Systematic access to managed chiropractic care not only may prove to be clinically beneficial but also may reduce overall health care costs.[14]
Not only did this study show chiropractic care reduced costs, it also showed a shift in patients to chiropractors from MDs when given the opportunity.
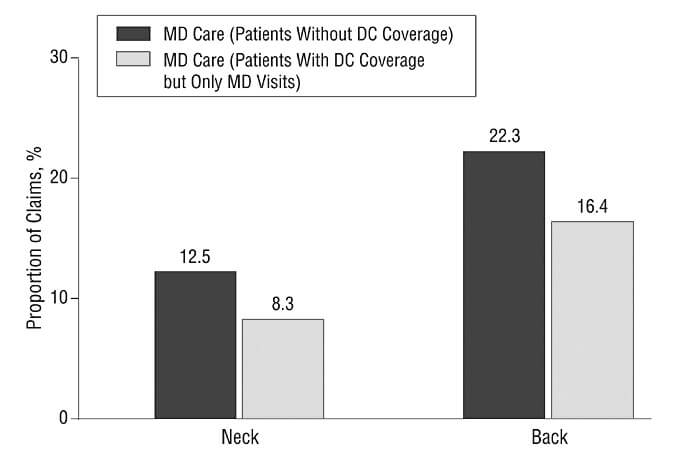
Figure 5. Medical care substitution. Presence of chiropractic coverage was associated with a shift in the case distribution away from medical doctors (MDs) to doctors of chiropractic care (DCs) for neck and back problems, indicating a substitution of chiropractic for physician care. All proportional differences are statistically significant at the P<.001 level.
Comments by the authors of this study were also divergent to Ward Casscell’s conclusion:
The high prevalence and recurrent incidence of back pain, as well as the heavy economic and disability burden that it imposes on society as documented in the literature, point to a major area of public health concern. Simultaneously, there is growing evidence for the low risks associated with chiropractic spinal manipulation in most cases and favorable evidence for its effectiveness in treating low back pain. In addition, patients treated for back pain by DCs tend to be more satisfied than patients treated by MDs. However, despite this evidence for safety, effectiveness, and growing public demand, health insurance coverage for chiropractic care continues to remain restricted, relative to other health services, particularly in the managed care sector.[15]
Casscells’ conclusion also contradicts the survey of ADSM that showed Service members preferred to select chiropractors over osteopaths or physical therapists (five being very likely), the response was again very positive with “responses from threes to fives.”[16]
Nonetheless, Dr. Casscells mentions in his cover letter of March 3, 2009, that “in the absence of chiropractic care, various comparative treatment options are available to active duty Service members, their families, and other beneficiaries of the Military Health System.” Dr. Casscells’ belief that chiropractic care is “comparable treatment” to osteopathic, medical, or physical therapy is hugely erroneous.
To the contrary, no one but chiropractors offer chiropractic care. What Dr. Casscells calls “comparative treatment options” are, in fact, not comparable. Various research studies confirm standard physical therapy is not equivalent to chiropractic spinal care, and to suggest it is completely misleading.
As well, the Evaluation of the TRICARE Program, Fiscal Year 2010 Report to Congress, also mentioned this erroneous comparison:
TRICARE does not cover chiropractic care, but family members may be referred to nonchiropractic health care services—physical therapy, family practice or orthopedics—for treatment as appropriate. http://www.tricare.mil/ChiropracticCare
Inexplicably, TRICARE has ignored the largest study done on acute low back pain in adults by the US Public Health Service’s Agency for Health Care Policy and Research. In 1994, AHCPR issued a 170-page study entitled “Acute Low Back Pain in Adults,” along with an accompanying 30-page “Quick Reference Guide for Clinicians” entitled “Acute Low Back Problems in Adults: Assessment and Treatment.”[17] A Patient Guide was also disseminated to the public with the same recommendations in laymen terms. This two-year study of 4,000 appropriate studies recommended spinal manipulation as a “proven treatment.” It also was very critical of spine surgery and medical methods in general.
The section on Spinal Fusion from the AHCPR’s Clinical Practice Guideline clearly summarized the research:
There appears to be no good evidence from controlled trials that spinal fusion alone is effective for treatment of any type of acute low back problems in the absence of spinal fractures or dislocation….Moreover, there is no good evidence that patients who undergo fusion will return to their prior functional level.[18]
What angered traditional medicine the most about the AHCPR study was its finding that confirmed the rare need for surgery except in the most severe cases that did not respond to conservative care. The following was stated in its Patient Guide, Understanding Acute Low Back Problems:
Even having a lot of back pain does not by itself mean you need surgery. Surgery has been found to be helpful in only 1 in 100 cases of low back problems. In some people, surgery can even cause more problems. This is especially true if your only symptom is back pain.
People with certain nerve problems or conditions such as fractures of dislocations have the best chance of being helped by surgery. In most cases, however, decisions about surgery do not have to be made right away. Most back surgery can wait for several weeks without making the condition worse.
If your health care provider recommends surgery, be sure to ask about the reason for the surgery and about the risks and benefits you might expect. You may also want to get a second opinion.[19]
The recommendations also upset the physical therapists. Standard forms of passive care by physical therapists were also not recommended for lower back pain. The Patient Guide published by the U.S. Public Health Service also states:
A number of other treatments are sometimes used for low back symptoms. While these treatments may give relief for a short time, none have been found to speed recovery or keep acute back problems from returning. They may also be expensive. Such treatments include: Traction, TENS, massage, biofeedback, acupuncture, injections into the back, back corsets, ultrasound.[20]
Subsequent studies have also shown medical primary care physicians and physical therapists are poorly educated and clinically inferior to the services of chiropractors for musculoskeletal disorders.
New studies have confirmed that most primary care physicians are inept in their training on musculoskeletal disorders,[21] more likely to ignore recent guidelines[22], and more likely to suggest spine surgery than surgeons themselves.[23] As well, biased physicians suffer from “professional amnesia”[24] when they inexcusably forget to inform patients that chiropractic care is a recommended option to the often ineffective medical methods.
In 1998, Kevin B. Freedman, MD, and Joseph Bernstein, MD, published a landmark study in Journal of Bone and Joint Surgery wherein they administered a validated musculoskeletal competency examination to recent medical graduates who had begun their hospital residency; 82 percent of these medical doctors failed to demonstrate basic competency on the examination, leading the authors to conclude, “We therefore believe that medical school preparation in musculoskeletal medicine is inadequate.” [25]
In their 2004 review published in Physician and Sports Medicine, Elizabeth A. Joy, MD, and Sonja Van Hala, MD, MPH, described the formal training of a sample of medical graduates. “The average time spent in rotations for courses devoted to orthopedics during medical school was only 2.1 weeks. One third of these examinees graduated without any formal training in orthopedics. As would be expected, these data suggest that limited educational experience contributes to poor performance.” [26]
Many physical therapists hold themselves out to be spine therapists, but a study by JD Childs et al.[27] on the physical therapists’ knowledge in managing musculoskeletal disorder (MSD) conditions found that only 21 percent of students working on their Master’s degree in physical therapy and 25 percent of students working on their doctorate degree in physical therapy achieved a passing mark on the Basic Competency Exam.
Even those physicians with a special interest in low back pain were more likely to believe in outdated concepts such as narcotics, complete bed rest, and avoidance of work are appropriate for acute low back pain—concepts now regarded as inappropriate. Oddly, there were no important differences in back pain beliefs between those with and without a special interest in musculoskeletal medicine.[28] It appears that any MD with an interest in back pain can hang out a “pain clinic” shingle even when poorly trained in this area.
The Bishop study published in Spine scored the content of the family physician-directed care and found it to be “highly guideline-discordant.” The three studies by Bishop et al. provide an excellent illustration of the slow pace of implementation of evidence-based spinal care into primary care settings.
“Typically, the family physician-based care involved excessive use of passive therapies such as massage and passive physical therapy, excessive bed rest, and excessive use of narcotic analgesics,” said Paul B. Bishop, DC, MD, PhD, Clinical Associate Professor in the Department of Orthopaedics at University of British Columbia. [29]
As well, RAND earlier had reported that 94 percent of all manipulative care was delivered by chiropractors, with osteopathic physicians delivering 4 percent, and general practitioners, physical therapists, and orthopedic surgeons accounting for the remainder.[30]
The research is clear that MDs, DOs, and PTs are not comparable spine specialists as Dr. Casscells suggests. Considering chiropractors have carried the banner of manipulative therapy since 1895 while, for the most part, the osteopaths relinquished this art in the early 1960s in order to be assimilated into the medical ranks, physical therapists have ignored this treatment to avoid the quackery stigma, and medical physicians have chosen to vilify this form of care, it is obvious that chiropractors are the professionals who lay claim by far to the most experience in manipulation, and rightfully so.[31]
Suspect Studies
In his report to Congress, Dr. Casscells gave an assessment of the health care benefits of chiropractic care from a few obscure minor research studies that, in my estimation, were poorly designed, small in size, and specifically selected to cast a bad light upon chiropractic care.
To my amazement, Dr. Casscells’ report failed to mention the major international and American studies that have proven the benefits of chiropractic care over medical care. The following is a review of the numerous international and American guidelines that recommend spinal manipulation for both acute and chronic low back pain:
- 1978: New Zealand Royal Commission on Chiropractic
- 1990: RAND study on appropriateness of spinal manipulation
- 1990: Meade Study (UK) comparing manipulation vs. hospital care
- 1993: Manga Report Ontario (Canada) Ministry of Health
- 1994: AHCPR Acute Low Back Pain Guideline
- 1994: Clinical Standards Advisory Group (UK)
- 1995: Council on Chiropractic Guidelines and Practice Parameters
- 2003: Ontario Workers’ Safety and Insurance Board
- 2003: Norway Spine Study
- 2004: European Back Pain Guidelines.
- 2004: The UK Back Pain Exercise And Manipulation (UK BEAM) Trial
- 2004: Swedish Lumbar Spine Study
- 2007: Guideline on Back Pain: American College of Physicians
- 2008: Decade of Bone & Joint Disorders: CLBP
- 2008: The Bone and Joint Decade Task Force on Neck Pain and Its Associated Disorders
- 2009: The National Institute for Clinical Excellence (UK-NICE)
As well, an editorial in the Annals of Internal Medicine published jointly by the American College of Physicians and the American Society of Internal Medicine (1998) noted that” spinal manipulation is the treatment of choice”:
The Agency for Health Care Policy and Research (AHCPR) recently made history when it concluded that spinal manipulative therapy is the most effective and cost-effective treatment for acute low back pain[32]. The 1994 guidelines for acute low back pain developed by AHCPR concluded that spinal manipulation hastens recovery from acute low back pain and recommended that this therapy be used in combination with or as an alternative to non-steroidal anti-inflammatory drugs. At the same time, AHCPR concluded that various traditional methods, such as bed rest, traction, and other physical and pharmaceutical therapies were less effective than spinal manipulation and cautioned against lumbar surgery except in the most severe cases.
Perhaps most significantly, the guidelines state that unlike nonsurgical interventions, spinal manipulation offers both pain relief and functional improvement. One might conclude that for acute low back pain not caused by fracture, tumor, infection, or the cauda equina syndrome, spinal manipulation is the treatment of choice. [33] (emphasis added)
The American College of Physicians and the American Pain Society published in 2007 a Joint Clinical Practice Guideline for the Diagnosis and Treatment of Low Back Pain that also recommended spinal manipulation for acute, chronic. or subacute low back pain. [34]
The American College of Occupational and Environmental Medicine (ACOEM) has revised its Occupational Medicine Practice Guidelines, which have not always taken a positive view of chiropractic manipulation. In fact, similar to what we now find with TRICARE, the second edition of the guidelines, released in 2005, was heavily criticized by some in the chiropractic community for bias and for ignoring the current research that endorses chiropractic care.[35]
ACOEM’s latest chronic pain guidelines now represent a step in the right direction in terms of recognizing the value of chiropractic care. The guidelines actually recommend manipulation for chronic, persistent low back or neck pain and cervicogenic headache.2 This is significant because in the past, the guidelines failed to recommend manipulation, even when other treatment strategies (medication, shots, surgery) were rated as less effective.
DoD Déjà Vue
In fact, this recent Chiropractic Care Study paralleled the DoD’s initial study, Chiropractic Health Care Demonstration Program (CHCDP), during the 1990s on chiropractic care[36]:
The National Defense Authorization Act for Fiscal Year 1995 mandated that Congress undertake a demonstration project to determine the cost effectiveness of adding chiropractic care in the military. That project became the Chiropractic Health Care Demonstration Program (CHCDP). The Department of Defense (DoD) directed the military to begin a three-year demonstration project (Aug. 1995 to Aug. 1998) at 10 military treatment facilities, with three other military sites not offering chiropractic used to compare outcome measures.
The CHCDP contractor, Birch & Davis, analyzed the CHCDP data and drafted a report, which was submitted to Congress by the DoD this February.
Among the conclusions by Birch & Davis:
- “Results of the survey data and referral patterns at each site suggest that traditional health care providers recognized the value of chiropractic care by their willingness to refer patients to chiropractic clinics.
- “Perceptions and attitudes about the acceptance of doctors of chiropractic and the appropriateness of spinal manipulation to treat certain medical conditions were judged to be favorable by traditional providers.
- “Provider attitudes toward doctors of chiropractic changed positively over time. The ability of doctors of chiropractic was judged more favorably after their integration. The study found that among traditional providers, the perceived appropriateness of chiropractic care and the perceived abilities of doctors of chiropractic increased over time.
- “Analysis of data collected from patients and providers indicates that chiropractic care was well received by the patient population. Overall, patients responded more favorably to chiropractic treatment than they did to traditional medical care.”
- “Chiropractic service appears to have complemented and augmented traditional medical care. Enhanced readiness and the likely benefit of improved retention rates provide additional support for the advisability of integrating chiropractic care into the MHS.
- “The CHCDP did not result in any adverse medical care or patient perceptions that would contraindicate the feasibility of offering chiropractic care to DoD beneficiaries throughout the military health system.”
The executive summary of the Birch/Davis report said it was “feasible to establish chiropractic services within the DoD,” but advised against implemented chiropractic in the military because it would cost, by their estimate, $70.9 million.
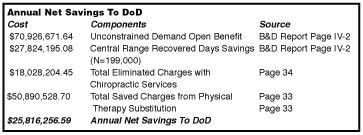
Chiropractic and civilian members of the CHCDP oversight committee filed their own report (Muse Report) to Congress, which was accepted instead of the DoD’s Birch/Davis report. The most crucial disagreement between the two reports is the cost of implementing chiropractic care in the military health care services. The Muse Report contends that those costs will be offset by inpatient care, emergency room services, physician services, physical therapy, surgical services, and recovered days; that these cost offsets will result in an “annual net savings to the DoD of $25.8 million.”
The following table from the Muse report tabulates those savings.
In both the original CHCDP study and the two recent reports on chiropractic care cited in the TRICARE study, once again this huge consideration was omitted: the amount of money and disability prevented by chiropractic care over spine surgery, passive physical therapy, primary care medications/opioids, or pain center epidural shots.
In the Casscells letter, he spoke of the added costs, but failed to mention the savings from chiropractic management rather than medical management of these back pain cases. A similar comparison done with Medicare statistics showed the favorable cost savings utilizing chiropractic care:
This study examines cost, utilization and effects of chiropractic services on Medicare costs. The study compared program payments and service utilization for Medicare beneficiaries who visited DCs and those who visited other types of physicians. The results indicated that chiropractic care could reduce Medicare costs. Medicare beneficiaries who had chiropractic care had an average Medicare payment of $4,426 for all Medicare services. Those who had other types of care had an average of $8,103 Medicare payment for all Medicare services. The per claim average payment was also lower with chiropractic patients, having an average of $133 per claim compared to $210 per claim for individuals who did not have chiropractic care.[37]
The aforementioned international studies also agree that chiropractic care is the better buy in back pain care. According to Pran Manga, PhD, Ontario (Canada) health economist, “There is an overwhelming body of evidence indicating that chiropractic management of low back pain is more cost-effective than medical management.” [38]
According to Dr. Manga:
The role and position of chiropractic care in the health care system must be transformed from being alternative and separate to alternative and mainstream. This transformation requires that chiropractic services become integrated in the many health care delivery organizations that collectively constitute the health care system. There is solid and impressive economic and related justification for the desired integration. Chiropractic care is a cost-effective alternative to the management of neuromusculoskeletal conditions by other professions. It is also safer and increasingly accepted by the public, as reflected in the growing use and high patient retention rates. There is much and repeated evidence that patients prefer chiropractic care over other forms of care for the more common musculoskeletal conditions.[39]
Despite the opinions of these studies, Dr. Casscells fails to mention them or the huge cost factor and has the audacity to suggest by omission there would be no cost savings whatsoever from chiropractic intervention. Instead, his analysis only mentions the potential cost of providing chiropractic added to rather than was a substitute for other medical services. His comparison showed that “making chiropractic available increases the total number of care visits by 4 to 10 visits per patient.” [40]
The authors of the Nelson et al. study also contradicted Casscells’ belief that chiropractic care would be an added expense:
This study found evidence that a substantial portion of the chiropractic care sought by the members with insurance coverage was more often substituted for medical care rather than add-on care.
The analyses related to NMS episodes elucidate sources of these cost savings relating to chiropractic treatment of common NMS complaints, such as neck and back pain. Focusing on low back pain diagnoses that were selected specifically for comparability between medical and chiropractic practice, our analysis found that patients with chiropractic coverage had significantly lower rates of use of resource-intensive technologies, such as x-ray examinations, MR image, and surgery, and lower use of more expensive patient care settings, such as inpatient care. This is reflected in the significantly lower cost, at both the episode level and the patient level, of providing care for back pain…In addition, the substitution of chiropractic for physician care evident from the shift in the case distribution between physicians and DCs when chiropractic coverage was present also contributed to the conservation of health care resources. [41]
The recent announcement of the addition of acupuncture illustrates the double standard in the MHS/TRICARE program. According to an article by Cheryl Pellerin, “Doctors Use Acupuncture as Newest Battlefield Tool,” Armed Forces Press Service, December 13, 2010, the bias against chiropractic was clear when it was left out:
And in June, the Army surgeon general released a report that recommended “a holistic, patient-centered approach” to pain management that uses all kinds of therapy, from conventional medicine to “complementary and alternative modes such as acupuncture, meditation, biofeedback, yoga and others.”
Considering chiropractic is the leader in CAM treatments, how can it be omitted from this article or from the MHS program unless there is either bias or ignorance of the research? For example, while this article praised acupuncture, the comparative research studies are not as boastful. According to a study by L. Giles and R. Muller, “Chronic Spinal Pain – A Randomized Clinical Trial Comparing Medication, Acupuncture and Spinal Manipulation,” acupuncture did not fare as well as chiropractic care.
Australian patients with chronic lower back pain of at least 13 weeks duration were randomly assigned either to medication, needle acupuncture or spinal manipulation. The results provided evidence that in patients with chronic spinal pain, manipulation results in greater short-term improvement than acupuncture or medication. The patients receiving spinal manipulation also reported a much higher full recovery rate (27%) than either the acupuncture (9%) or the medication (5%).[42]
Once again we see the MHS has ignored the research that promotes chiropractic care and chooses to use less effective methods. Perhaps one factor in this acupuncture program was the acupuncturists were MDs, which may have paved the way for its implementation. Even one medical acupuncturist asked the obvious question:
“The question that comes to my mind is,” Air Force Col. (Dr.) John Baxter said, “if you can make the majority of patients better during their clinic visit without medicines, then why are you still treating patients the old way?
Perhaps another question needs to be asked: why is the MHS/TRICARE ignoring the best form of treatment for back pain, i.e., chiropractic care, and “treating patients the old way?”
Wither on the Vine
Dr. Casscells’ opinion that other types of practitioners can offer the chiropractic benefit appears to be yet another fight by the medical bureaucrats to have chiropractic wither on the vine in its illegal attempt to boycott the chiropractic profession. We’ve seen this before when Sec. Donna Shalala of HHS issued a formal “Policy Letter” proclaiming physical therapists, MDs and DOs could perform the chiropractic service.
This fight concerned Medicare Part C, which came into existence with the passage of the 1997 Balanced Budget Act. Part C was essentially Medicare’s managed care plan, administered by the Health Care Financing Administration (HCFA), department of Health and Human Services.
The ACA’s suit against HHS was originally filed in November 9, 1998 in response to then-new HHS guidelines that essentially excluded chiropractic services from the Medicare managed care program. Specifically, the guidelines allowed managed care plans that belonged to the Medicare+Choice program to substitute the services provided by doctors of chiropractic, including the ability to perform “manual manipulation of the spine to correct a subluxation.”[43]
Ironically, after decades of saying spinal subluxations were imaginary, that manipulation was ineffective and dangerous, while ignoring the poor education and lack of training of MDs in this healing art, now the medical profession decided that MDs, DOs, and PTs could offer this service as well as chiropractors. In fact, their goal was not to enter into this field but to let it wither on the vine from disuse.
Mr. George McAndrews, attorney for the chiropractors, spoke of this irony in an interview in Chiropractic Economics, a trade journal:
Up until that time [before the Wilk victory], it was like dealing with a leper. After the injunction–which still exists–the battle turned to money. After declaring chiropractic to be a bastard child and then seeing it grow up to be an Einstein, everyone has tried to claim it as its own.
They all claim that [chiropractic is] part of the core of the universal practice of medicine. And physical therapists, who have never been trained like doctors of chiropractic, are now asserting the right to manually correct subluxations. Even osteopaths, who have never used subluxation, claim to be chiropractors at heart. Everyone wants a piece of the action.[44]
The irony of Dr. Casscells’ belief that chiropractic would increase costs is a ruse to boycott chiropractic care. Studies have repeatedly shown chiropractic is faster, cheaper, and safer, but Casscells seems to ignore this research. Instead, he suggests this service can be offered by non-chiropractors. Again, this is reminiscent to Shalala’s decision that was overturned by court.
On January 15, 2002 there was a revision to the “Operational Policy Letter” originally issued in 1994 in which Medicare’s Center for Beneficiary Choices wrote:
“The (Medicare) statute specifically references manual manipulation of the spine to correct a subluxation as a physician-level service. Thus, Medicare+Choice organizations must use physicians, which include chiropractors, to perform this service. They may not use non-physician physical therapists for manual manipulation of the spine to correct a subluxation.” [45] (emphasis added.)
Without question the most ironic, hypocritical, and disingenuous regulation in Medicare by the Health and Human Services bureaucrats under Sec. Shalala was the decision that the unique and hard fought right for patients to have access for chiropractic care could be supplied by those whose associations that were diametrically opposed to it–medical physicians and physical therapists.
In its Dec. 13, 2005 decision, the three-judge appeals panel overturned the District Court’s ruling, noting that the District Court lacked the jurisdiction to decide whether medical doctors and osteopaths may manipulate the spine to correct subluxations. The appeals panel also raised an important point on the issue of which health care providers are qualified to provide chiropractic services, not just which providers are licensed to provide such services:
“The regulation states that ‘[i]f more than one type of practitioner is qualified to furnish a particular service, the HMO may select the type of practitioner to be used.’ The HMO’s invocation of this provision would squarely present the question whether medical doctors and osteopaths, as well as chiropractors, are ‘qualified to furnish’ the service of manual manipulation of the spine to correct a subluxation.”[46]
Then-ACA President Richard Brassard, DC, remarked about this decision;
The ACA is extremely pleased that the District Court’s ruling allowing MDs and DOs to provide a uniquely chiropractic service was nullified. We are happy that the issue is now whether or not a practitioner is ‘qualified,’ not whether or not a practitioner is simply licensed. The ACA’s position has been and remains that only chiropractors are qualified by education and training to correct subluxations. Because of the Appeals Court’s decision, chiropractors can continue to fight to safeguard their right to be the sole providers of this service, and to ensure Medicare patients’ rights to access doctors of chiropractic.[47]
Conclusion
While most patients are not candidates for disc surgery, they are candidates for spinal manipulation. Unfortunately, too many unsuspecting back pain patients are denied chiropractic care and are routinely railroaded into spine surgeries despite the proof to the contrary. This oversight is perplexing considering the huge costs of medical care for low back pain as noted in the international studies. I can only guess that Casscells’ omission of this major cost savings may be due to his medical bias against chiropractors.
The proof is positive and research studies cannot be clearer that chiropractic stands at the top of spinal treatments as Anthony Rosner, PhD, testified before The Institute of Medicine: “Today, we can argue that chiropractic care, at least for back pain, appears to have vaulted from last to first place as a treatment option.”[48]
I believe the facts are clear: the active military and TRICARE recipients of chiropractic care have rated chiropractic at the top of their patient satisfaction rates; the MTF unit personnel were also very pleased with their chiropractic programs; and the potential cost savings is obvious over medical care as the CHCDP report indicated a savings of nearly $26 million annually to the DoD, another omission in the Casscells report.
The biggest obstacle now are the medical personnel in the DoD who attempt to ignore the wish of Congress to implement chiropractic care with their poorly supported conclusions as Dr. S. Ward Casscells has shown.
This conflict is similar to the objections of the chiropractic profession when the CHCDP conclusions did not “adequately reflect the advisability of including chiropractic services.”
The chiropractic members of the oversight committee did not believe that they were afforded “sufficient opportunity for input during the course of the CHCDP, nor was their involvement sought in the analysis of CHCDP data or preparation of the draft final report as mandated by Congress…the chiropractors of the oversight advisory committee clearly felt that the report did not “adequately reflect the advisability of including chiropractic services.”[49]
I believe the same can now be said of Dr. Casscells’ opinion. The data supports the need for chiropractic care and the surveys indicate high patient satisfaction rates. The glaring omission of the cost savings of chiropractic care over medical care mentioned by Nelson and Manga was a serious oversight that should have been included in these studies. As well, the lack of any chiropractic input into these studies seem eerily reminiscent to the original Medicare legislation when medical opponents tampered with the committee.
The skewed conclusion by S. Ward Casscells, MD, reflects the “wither on the vine” strategy of the AMA’s Committee on Quackery that was exposed in the Wilk et al. v. AMA et al. antitrust trial.[50] The medical executives told the court that chiropractic was quackery, unscientific, and dangerous. Under oath, however, they had no proof whatsoever to substantiate their claims as the judge noted in her decision in favor of the chiropractor-plaintiffs.
Today, it appears again we see the same “wither on the vine” tactic by the TRICARE administration that chose to misinterpret the findings, overlook the obvious positives about chiropractic care, and jump to conclusions not supported by facts.
Just as chiropractic members of the CHCDP oversight committee filed their own report to congress, it is imperative that the same should be done with this TRICARE report. TRICARE is too big to leave the exclusion of chiropractic spinal care to the whims of medical opponents who wish to see chiropractic wither on the vine.
Considering the comparative studies showing the superiority of chiropractic care to medical care, it appears TRICARE and Dr. Casscells goal is to deprive patients of the benefit from spinal manipulation as practiced by doctors of chiropractic, and to deprive doctors of chiropractic of the opportunity to treat those patients based on insufficient evidence. Indeed, medical bias is the underlying problem with this issue.
The present policy of TRICARE to limit chiropractic care smacks of the same boycott strategy that led to the Wilk v. AMA antitrust suit. As I’ve indicated, TRICARE has ignored favorable research studies supporting chiropractic care is faster, safer, more effective and less costly than anything the medical world has to offer. The fact that TRICARE is willing to promote acupuncture as a medical service despite the proof that chiropractic care is more effective illustrates the bias among the TRICARE medical bureaucrats.
I believe the TRICARE decision making process demands reevaluation and transparency due to the lack of chiropractic advocates in this obvious illogical conclusion to contain the expansion of chiropractic care.
CC: Dr. S. Ward Casscells
Senator Saxby Chambliss
Senator Johnny Isakson
Representative Austin Scott
American Chiropractic Association
Association of Chiropractic Colleges
[1] Chiropractic Care Study, Senate Report 110-335 accompanying the National Defense Authorization Act for FY 2009; letter sent to Congressmen by Ellen P. Embrey, Deputy Assistant Secretary of Defense (September 22, 2009):2.
[2] Ibid. p. 3.
[3] Ibid.
[4] Ibid.
[5] C. Richard Wolf, “Industrial Back Injury,” International Review of Chiropractic, 26 (1974):6-7
[6] S. Ward Casscells, letter to Congressmen, “Chiropractic Care Study,” (2009):3
[7] J Jordan, et al., “Herniated Lumbar Disc,” BMJ Clinical Evidence, quote in The BACKLETTER® 25/7 (July 2010):76-77
[8] P Manga, ibid.
[9] SJ Bigos, O Bowyer, G Braea, K Brown, R Deyo, S Haldeman, et al. “Acute Low Back Pain Problems in Adults: Clinical Practice Guideline no. 14.” Rockville, MD: U.S. Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research; 1992. AHCPR publication no. 95-0642.
[10] MS Micozz, “Complementary Care: When Is It Appropriate? Who Will Provide It?” Annals of Internal Medicine 129/1 ( July 1998):65-66
[11] B McClain, “Mainstream Makes Adjustment,” The Washington Post, (July 17, 2007).
[12] RA Deyo, “Low -Back Pain,” Scientific American, (August 1998):49-53
[13] G Waddell and OB Allan, “A Historical Perspective On Low Back Pain And disability, “Acta Orthop Scand 60 (suppl 234), (1989)
[14] Craig F. Nelson, DC, MS, Antonio P. Legorreta, MD, MPH; R. Douglas Metz, DC;; Saurabh Ray, PhD; Helen Oster Chernicoff, MD, MSHS; Nicholas A. DiNubile, MD, “Comparative Analysis of Individuals With and Without Chiropractic Coverage Patient Characteristics, Utilization, and Costs,” Arch Intern Med. 164/18 (2004):1985-1992
[15] Ibid.
[16] Ibid.
[17] Bigos et al. US Dept. of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research, Clinical Practice Guideline, Number 14: Acute Low Back Problems in Adults AHCPR Publication No. 95-0642, (December 1994)
[18] S Bigos, ibid. p. 90.
[19] S Bigos, ibid. p. 8.
[20] Ibid.
[21] EA Joy, S Van Hala, “Musculoskeletal Curricula in Medical Education– Filling In the Missing Pieces, The Physician And Sports Medicine,” 32/11 (November 2004).
[22] PB Bishop et al., “The C.H.I.R.O. (Chiropractic Hospital-Based Interventions Research Outcomes) part I: A Randomized Controlled Trial On The Effectiveness Of Clinical Practice Guidelines In The Medical And Chiropractic Management Of Patients With Acute Mechanical Low Back Pain,” presented at the annual meeting of the International Society for the Study of the Lumbar Spine Hong Kong, 2007; presented at the annual meeting of the North American Spine Society, Austin, Texas, 2007; Spine, in press.
[23] SS Bederman, NN Mahomed, HJ Kreder, et al. In the Eye of the Beholder: Preferences Of Patients, Family Physicians, And Surgeons For Lumbar Spinal Surgery,” Spine 135/1 (2010):108-115.
[24] A Rosner, “Evidence or Eminence-Based Medicine? Leveling the Playing Field Instead of the Patient,” Dynamic Chiropractic, 20/25 (November 30, 2002)
[25] KB Freedman, J Bernstein, “The Adequacy Of Medical School Education In Musculoskeletal Medicine,” J Bone Joint Surg Am. 80/10 (1998):1421-7
[26] Joy ibid.
[27] JD Childs, JM Whitman, PS Sizer, ML Pugia, TW Flynn, A Delitto, “A Description Of Physical Therapists’ Knowledge In Managing Musculoskeletal Conditions,” BMC Musculoskelet Disord 6 (2005):32.
[28] R Buchbinder, M Staples, D Jolley, “Doctors With a Special Interest in Back Pain Have Poorer Knowledge About How to Treat Back Pain,” Spine, 34/11 (May 2009)
[29] Bishop, ibid.
[30] PG Shekelle, AH Adams, MR Chassin, E Hurwitz, RE Park, RB Phillips, RH Brook, “The Appropriateness of Spinal Manipulation for Low-Back Pain: Project Overview and Literature Review,” RAND (1991):3. Santa Monica, Calif.
[31] Ibid.
[32] SJ Bigos, O Bowyer, G Braea, K Brown, R Deyo, S Haldeman, et al. “Acute Low Back Pain Problems in Adults: Clinical Practice Guideline no. 14.” Rockville, MD: U.S. Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research; 1992. AHCPR publication no. 95-0642.
[33] MS Micozz, “Complementary Care: When Is It Appropriate? Who Will Provide It?” Annals of Internal Medicine 129/1 ( July 1998):65-66
[34] R Chou, et al., “Diagnosis and Treatment of Low Back Pain: A Joint Clinical Practice Guideline from the American College of Physicians and the American Pain Society,” Low Back Pain Guidelines Panel, Annals of Internal Medicine 2 147/7 (October 2007):478-491
[35]Lewkovich G, Haneline M, Mumbauer E, Sackett M. “The ACOEM Occupational Medicine Practice Guidelines: Biased Against Chiropractic Care.” Dynamic Chiropractic, Jan. 1, 2005.
[36] Editorial Staff, “Report to Congress on Chiropractic in the Military: Feasible, but not Advisable,”
|
Dynamic Chiropractic 18/09 ( April 17, 2000) |
|
[37] “Utilization, Cost, and Effects of Chiropractic Care on Medicare Program Costs,” by Muse and Associates. American Chiropractic Association, 2001.
[38] P Manga, D Angus, C Papadopoulos, W Swan, “The Effectiveness and Cost-Effectiveness of Chiropractic Management of Low Back Pain,” (funded by the Ontario Ministry of Health) (August, 1993):104
[39] Pran Manga, PhD, “Economic case for the integration of chiropractic services into the health care system,” 23(2) (Feb 2000): 118-22.
[40] Report to Congress, p. 8
[41] Antonio P. Legorreta, MD, MPH; R. Douglas Metz, DC; Craig F. Nelson, DC, MS; Saurabh Ray, PhD;Helen Oster Chernicoff, MD, MSHS; Nicholas A. DiNubile, MD, “Comparative Analysis of Individuals With and Without Chiropractic Coverage Patient Characteristics, Utilization, and Costs,” Arch Intern Med. 2004;164:1985-1992
[42] L. Giles and R. Muller, “Chronic Spinal Pain – A Randomized Clinical Trial Comparing Medication, Acupuncture and Spinal Manipulation” Spine 2003; 28:1490-1503
[43] Michael Devitt, “Landmark Decision in ACA Lawsuit Against HHS,” Dynamic Chiropractic 24/02 (January 15, 2006)
[44] Linda Segall, “Chiropractic in distress!” Chiropractic Economics, Issue 5 (April 2003)
[45] Editorial Staff, “No More Using PTs to Correct Subluxations,” Dynamic Chiropractic 20/06 (March 11, 2002)
[46] Michael Devitt, “Landmark Decision in ACA Lawsuit Against HHS,” Dynamic Chiropractic 24/02 (January 15, 2006)
[47] ibid.
[48] Testimony before The Institute of Medicine: Committee on Use of CAM by the American Public on Feb. 27, 2003.
|
[49] Editorial Staff, “Report to Congress on Chiropractic in the Military: Feasible, but not Advisable,” Dynamic Chiropractic 18/09 ( April 17, 2000) |
|
[50] Chester A. Wilk, James W. Bryden, Patricia A. Arthur, Michael D. Pedigo v. American Medical Association, Joint Commission on Accreditation of Hospitals, American College of Physicians, American Academy of Orthopaedic Surgeons, United States District Court Northern District of Illinois, No. 76C3777, Susan Getzendanner, Judge, Judgment dated August 27, 1987.