A Chiropractic Proposal
for the
Governor’s Advisory Council
on Workers’ Compensation
by
JC Smith, MA, DC
Representative of the Georgia Chiropractic Association
&
Smith Spinal Care Center
1103 Russell Parkway
Warner Robins, GA 31088
Objective: To lower workers’ compensation costs with the greater utilization of chiropractic care.
Background: Musculoskeletal disorders (neck, back, wrist pain), a.k.a. MSDs, constitute an expensive epidemic in the workplace and in the general society, costing $50-75 billion dollar in the US alone.[1] Studies have shown chiropractic care to be safer, quicker, less-expensive with higher patient satisfaction rates than medical methods, including back surgery.[2] In light of these numerous studies and governmental recommendations showing the cost and clinical-effectiveness of spinal manipulative therapy (SMT) for low-back problems, a gross under-utilization of chiropractic care in Georgia’s workers’ comp (WC) program still exists, costing employers added lost work days for injured employees and increased WC insurance premiums. It also denies the injured-worker their legal right of making an informed consent as to current standards of care.
Chiropractic care in the Georgia workers’ compensation program has decrease by 70% in the last few years, now comprising less than one percent of the provider costs.[3] Although Georgia’ WC law allows for chiropractic care, injured-workers are denied this care due to many reasons:
1) the personal bias of some personnel directors,
2) refusal to be referred by medical gatekeepers,
3) PI attorneys who prefer surgery to attain higher medical costs for larger settlements,
4) and WC insurance companies which discourage the use of inexpensive chiropractic care in order to keep premiums as high as possible.
Conclusion: The full integration, direct-access of chiropractic care into the WC program would substantially lower healthcare costs. Studies have shown direct access to DCs lowers costs for MSDs compared to medical management.[4] If the goal of WC Board is to decrease expenses, rather than cutting back on chiropractic care as the recent trend has shown, I recommend the Board instead look at the ineffective, costly and often unnecessary back surgeries that fly in the face of the federal guidelines and recent research from around the world. I also recommend DCs to be on every panel of providers, and second opinions by DCs should be done before back surgery, as per the US federal guideline on acute LBP.[5]
Introduction
While sitting at a nice hotel on beautiful Jekyll Island may not be the perfect place to broach a serious issue concerning waste and abuse within the state’s workers’ comp program, on the other hand, the Governor’s Advisory Council is the appropriate place to make waves and to raise a few important questions that could save money and improve injured-workers’ clinical outcomes.
It is my contention that the insidious boycott of chiropractic care in Georgia’s workers’ compensation program has cost employers millions of dollars in added costs as well as denying injured workers their right to a choice in their own healthcare matters. Furthermore, this virtual boycott of chiropractic and the ever-present negative remarks by WC insurance adjusters leads one to believe there exists a form of professional profiling to exclude doctors of chiropractic from gaining more access to this marketplace.
Although I am a 22-year practitioner in Warner Robins operating a nationally-certified chiropractic rehabilitation facility in the state, I can count on one hand the number of WC cases I’ve had. When I’ve asked business-owners who are my patients about being placed on their panel of physicians, I am told that the WC insurance companies won’t allow it. When injured workers come to my office, most are denied authorization by their personnel directors. Most often, these injured workers are also lied to, being told that WC doesn’t cover chiropractic care. Indeed, as any doctor of chiropractic can attest, WC in our state is a closed-shop.
I contend, and the research will show, that the consequence of this boycott of chiropractors has led to increase in lost work days, medical and disability costs, increased insurance premiums for employers and, more so, it has denied injured workers their right to make an informed decision in regards to their own bodies. For those of us who’ve seen this sad situation firsthand, it illustrates the consequences when there is not a free market with fair competition at work in healthcare.
Instead, what exists today is a virtual medical monopoly which has dominated this market to the near exclusion of all competition. Indeed, without open competition in healthcare, abuse, waste, high costs and fraud continue unabated even in light of the recent research and recommendations that endorse spinal manipulative therapy for the vast majority of back and neck problems.
If the goal of Georgia’s WC Board is to lower health care costs while providing clinically-effective care in a controlled environment, I urge the Board to follow the guidelines and recommendations of governmental researchers from the US, UK, Canada, and Denmark. The homework has been done, now let’s implement them in our state.
This will require a paradigm shift from the old medical model to the new model of conservative care espoused in these guidelines. While medical detractors may object to my suggestions, I will let the experts and their research argue my case for me. The facts are clear that SMT is the superior method for the majority of low back and neck cases.
If the WC Board believes, as the experts profess, that evidence-based procedures from proven clinical and cost-effective methods are the best approach to improve outcomes and lower costs in the WC program, I’m certain this information will prove my case, save money for employers and taxpayers, improve clinical outcomes for injured workers and, generally, improve the WC program in our Peach State.
Outline of 12 Issues to be Discussed
To make my case, let me discuss twelve important issues that must be resolved in order to allow chiropractic care to lower costs and benefit injured workers:
1) A Case for Chiropractic Care page 5
2) You Don’t Slip Discs, But You Do Slip Joints 6
3) Distributive Injustice for Chiropractors 8
4) Dwindling Chiropractic Care in Georgia: The Facts 9
5) Perverse Motivations by WC Insurance & PI Attorneys 11
6) Bias in the Workplace 12
7) Role of Guidelines 13
8) Back Pain Guidelines from Denmark 15
9) Chiropractic Proposal to Save Money and Lost Work Days 16
10) Failed Back Surgery—Throwin’ Good Money In After Bad 18
11) Informed Consent—Quiz Your Doctor 20
12) Recommendations 22
1) A Case for Chiropractic Care
Let me set the table with a look at some facts. (For complete references, I refer you to my book, “How to Avoid Back Surgery: Chiropractic—the Proven Method for Back Pain”):
1) According to OSHA, the most frequently occurring on-the-job injuries are musculo-skeletal disorders (MSDs) in nature, specifically low back, neck and wrist disorders. The large number of musculoskeletal disorders — 647,000 MSDs resulting in at least one day away from work in 1996, according to Bureau of Labor Statistics (BLS) data is largely explained by the continued reliance on unassisted lifting, carrying, and pushing/pulling of loads; the increasing specialization of work; and the faster pace of work. [6]
2) Paul Shekelle, MD director of the RAND study on low-back problems: “To say that there is no scientific proof [of SMT], I would say that there’s considerably more randomized controlled trials which show benefit for this than there is for many other things which physicians and neurosurgeons do all the time.”[7]
3) According to the Agency for Health Care Reform & Policy (AHCPR) of the US Public Health Service, their 1994 federal guideline on acute low back pain in adults recommends spinal manipulation as a “proven treatment.” [8]
4) The AHCPR report also states that “Surgery has been found to be helpful in only one in 100 cases of low back problems.”[9]
5) The AHCPR recommendations also comment about standard physical therapy modalities: “While these treatments may give relief for a short time, none have been found to speed recovery or keep acute back problems from returning. They may also be expensive.”[10]
6) According to the 1994 British study on low back pain, “Traditional medical treatment has failed to halt this epidemic and may have contributed to it. There is a clear need to reconsider our whole approach to the management of low back pain and disability.”[11]
7) According to Dr. Gordon Waddell, orthopedist/researcher, “Low back pain is a 20th century healthcare disaster.”[12]
8) According to Dr. Pran Manga, Ph.D. and medical economist, “On the evidence, particularly the most scientifically valid clinical studies, spinal manipulation applied by chiropractors is shown to be more effective than alternative [medical] treatments for low back pain.”
9) According to Dr. Scott Boden, orthopedist/researcher, “the disc might not be the cause of pain. And if so, fixing it is a waste.” [13]
10) According to BE Finneson, PhD, 50 – 90% of the 300,000 disc surgeries done each year for ruptured discs are unnecessary and ineffective.[14]
11) According to WH Kirkaldy-Willis, MD and David Cassidy, DC, discs are involved in fewer than 10% of back pain cases.[15]
12) According to Nikolai Bogduk, MD, PhD, disc are involved in fewer than 5% of these cases.[16]
13) According to V. Mooney, MD, discs problems account for less than 1% of these cases.[17]
14) Low back pain alone accounts for 16 percent of all workers’ compensation claims but 33 percent of all WC costs.[18]
15) According to Met Life statistics, for the same diagnostic code for acute LBP, a chiropractic case cost them $800, a PT case $7,000 and a surgical case was $14,000+.[19]
16) According to RAND research, the rate of clinical iatrogenesis for DCs is 1-2 accidents per million treatments, 3 in 10 million morality rate. Adverse NSAIDs reactions caused 16,500 deaths annually; for surgery, the rate is 15,600 (morbidity) and 6,900 (mortality) per one million each year. [20]
17) Rene Cailliet, MD and author of many books on neck and back pain, “With all these [LBP therapies] and many more being used, it is apparent that most are not, per se, effective.”[21]
18) And my personal favorite: According to Robert Mendelsohn, MD, “Anyone who has a back surgery without seeing a chiropractor first should also have his head examined.”[22]
2) You Don’t Slip Discs, But You Do Slip Joints
Obviously the most recent LBP research done here in the US and abroad indicate conclusively that the traditional medical beliefs and treatments for LBP are inappropriate in the vast majority of cases. In other words, “slip discs” and “pulled muscles” are not the primarily causes of acute LBP, nor are back surgery, ultrasound and hot packs always the best forms of care. Research now has proved that the long-held belief in the disc theory for back pain is now dead.
Research now shows that most back pain is mechanical/functional in nature, that is, dysfunctional or misaligned spinal joints cause the pain and spasm associated with LBP. Joint Complex Dysfunction (JCD) causing neurophysiological and pathophysiological problems is now considered the most accurate explanation of mechanical low back pain.[23] Considering there are 137 joints in the human spine, one can easily understand this point that most LBP stems from joint problems and, thus, why spinal manipulation has worked so well to solve this epidemic.
In fact, experts tells us that disc abnormalities are not the primary source of pain in most LBP cases. Recent MRI studies which have shown the presence of disc abnormalities whether or not back pain exists have caused many experts to question the validity of MRI exams and spinal fusion.[24] Indeed, much of the problem with failed back surgery syndrome is the underlying JCD that has not been corrected.
Although this disc theory for back pain has been disproved by medical experts, this extremely expensive procedure is the focal procedure that continues unabated in Georgia’s WC program today. One solution to this is to establish clear guidelines for the WC program and to disseminate them throughout the state.
According to the US federal guideline:
“Degenerative discs, bulging disc and even herniated discs are part of the aging process for the spine and may be irrelevant findings: they are seen on imaging tests of the lumbar spine in a significant percentage of subjects with no history of low back problems. Therefore, abnormal imaging findings seen in a patient with acute low back problems may or may not be related to that individual’s symptoms.[25]
“Patients with acute low back pain alone, without findings of serious conditions or significant nerve root compression, rarely benefit from a surgical consultation. Many patients with strong clinical findings of nerve root dysfunction due to disc herniation recover activity tolerance within one month; no evidence indicates that delaying surgery for this period worsens outcomes. With or without an operation, more than 80% of patients with obvious surgical indications eventually recover.”[26]
Richard Deyo, MD and noted researcher, recently published in the Scientific American titled “Low-Back Pain.”[27] He mentions “Calling a physician a back-pain expert, therefore, is perhaps faint praise–medicine has at best a limited understanding of the condition. In fact, medicines’ reliance on outdated ideas may have actually contributed to the problem.” He continues to criticize “Old concepts supported only by weak evidence,” and the reliance on MRI exams to infer disc abnormalities as the cause of back pain. “Detecting a herniated disk on an imaging test therefore proves only one thing conclusively: the patient has a herniated disk.”
Not only does Dr. Deyo bash many medical concepts and treatments for back pain, he then mentions chiropractic as a possible solution, “Chiropractic is the most common choice, and evidence accumulates that spinal manipulation may indeed be an effective short-term pain remedy for patients with recent back problems.”
The AHCPR federal guideline on acute low back pain in adults is the most definitive study ever done on this subject. This 23-member panel of back experts headed by an orthopedic surgeon conducted a two-year study of 4,000 articles from the National Library of Medicine and recommends three initial treatments as “Proven Methods” for acute low back pain:
1) NSAIDs instead of pharmaceuticals
2) Ice/heat
3) Spinal manipulative therapy
After 2-4 weeks of this conservative care, unresponsive patients are then referred on for a surgical consultation.
This guideline advice and their clinical algorithm has been ignored within the Georgia WC program for no known good reasons other than to maintain the expensive status quo medical system. Indeed, when the US federal guideline states that “Surgery has been found to be helpful in only one in 100 cases of low back problems,” something is amiss when injured-workers are routinely routed initially to the surgeons here in Georgia and denied access to conservative chiropractic care.
This paradox begs the question: Just what good are research studies and governmental recommendations and guidelines if they are ignored? This question was answered by a member of the AHCPR panel, Richard Deyo, MD, MPH, University of Washington Medical School, recently co-authored in The New England Journal of Medicine an article, “The Messenger Under Attack–Intimidation of Researchers by Special Interest Groups.” He wrote that “The huge financial implications of many research studies invite vigorous attack… Intimidation of investigators and funding agencies by powerful constituencies may inhibit important research on health risks and rational approaches to cost-effective health care.” [28]
In fact, this is exactly what we’ve encountered with the implementation of the guideline on acute low back pain in adults here in Georgia.
3) Distributive Injustice for Chiropractors
In this light, the present WC guideline for back pain and MSDs are woefully outdated clinically, inadequate standards of care, a waste of tax money, and it denies patients access to the best care possible. This has led to increased costs for employers and increased unsuccessful outcomes for patients. It also has denied doctors of chiropractic the right to compete on a level playing field, a concept Dr. Pran Manga, medical economist, refers to as “distributive justice.”
“We would argue that the principle of distributive justice, and a parallel principle of equality of opportunity, require that the government implement all cost-effective substitutions; failure to do so results in unfairness to the taxpayers and unfairness to certain health care professionals…The monopolization of the health care services turf is also inequitable from yet another perspective. It denies some professions equal opportunity to earn income commensurate with their ability, effectiveness and effort…Inefficient use of health human resources is not just economically wasteful, it is also inequitable and generates higher levels of taxation…Equity is likely to become more important as the struggle over the health care turf becomes fiercer, and as taxpayers demand even greater value for the taxes they pay.”[29]
In fact, the 1997 Georgia WC statistics posted on the SBWC web page revealed this very point of distributive injustice only too clearly:
Physician Benefits: $70,066,443
Physical Therapy: $13,410,394
Chiropractic: $488,027
Shocking, isn’t it? Of this 1997 total for total provider (MD, PT, DC) expenses, $83,964,864, chiropractic incurred only $488,027, which equates to less than 1% of these costs; actually it figured out to be 0.58%. Again, considering back problems are the leading on-the-job injuries and SMT is acknowledged as a “proven method,” isn’t it very strange that chiropractic back experts are so under-utilized and paid for less than one percent of these monies?
An even more shocking example of the boycott of chiropractic care in the WC program is revealed by a computer analysis from the Georgia Board of Workers’ Compensation for “Back Injuries” for 1999. This 57 page report indicated that of the 2,829 cases reported in 1999, chiropractic had a total of only 81 cases, a mere 2.8% of these cases. More revealing facts for the discrepancy in monies paid to providers showed:
Physician Benefits: $4,640,602
Physical Therapy: $970,112
Chiropractic: $74,475
Of this total of $5,685,189, the chiropractic costs were 1.3%. Considering that MSDs are the largest injuries and manipulation is the preferred choice of treatment, it appears odd that chiropractic earned such a small amount of the pie.
Another example of distributive injustice is shown by the 1999 statistics for 284 cases of carpal tunnel syndrome, a.k.a., wrist pain, which is responsive to manipulation:
Physician Benefits: $581,812
Physical Therapy: $85,252
Chiropractic: $204
Of the total $667,268 paid for providers, chiropractic costs accounted for only .03%.
4) Dwindling Chiropractic Care in Georgia’s WC Program
In three short years, the WC program’s institutional bias was able to cut chiropractic claims by over 70% with the virtual boycott of our care for injured workers.[30] The biggest irony of this is the fact that for the same diagnostic codes for acute low back pain, chiropractic has been shown to be faster, safer and cheaper.[31] By avoiding the full implementation of chiropractic care, the WC program is costing taxpayers and business owners much more money than need be.
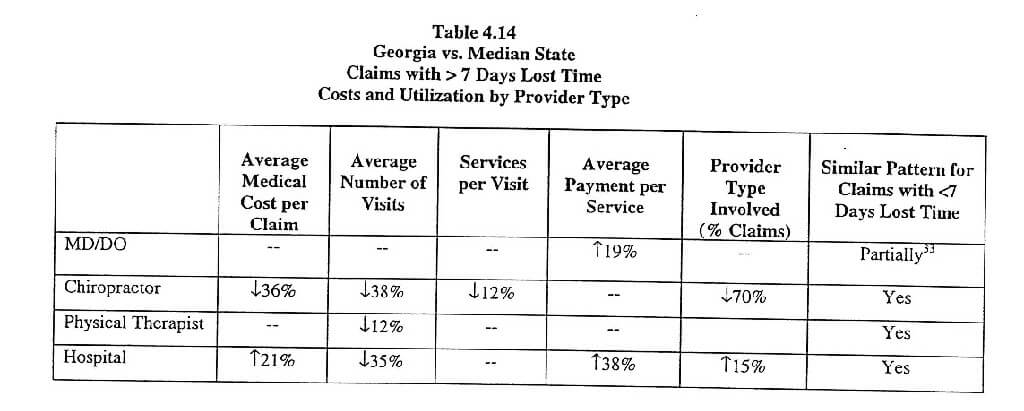
To prove my point that chiropractic care in Georgia has been severely limited, let me quote directly from a new comprehensive report of WC programs in 8 states, including Georgia, by the Workers Compensation Research Institute titled, “The Anatomy of Workers’ Compensation Medical Costs and Utilization: A Reference Book.” [32]
1) Georgia’s average claims cost is 20% higher than the median due to an average payment per service that is among the highest in the 8 states polled.
2) Chiropractors are involved in substantially fewer claims (-70%) than is typical and the average payments made to chiropractors when they are involved in a claim is also substantially lower (-36%). This is a function of lower utilization, in particular, fewer visits per claim (-38%).
3) Limits on chiropractic services (-12%) set in Georgia’s fee schedule may contribute to this outcome.
On the other hand, the medical statistics in WC claims are higher than the median.
1) The average payments per service paid to MD/DOs and hospitals is significantly higher in Georgia than is typical, however, this is offset in each case by lower utilization, particularly for hospitals.
2) The maximum fee levels set by Georgia’s fee schedule is somewhat higher than typical, particularly for surgical services (minor surgery +60.2%; major surgery +20%)
3) While the average costs per claim for office visits tend to be lower in Georgia compared to other states, costs for surgery are higher. For surgery, it is a higher per service payment that contributes to the higher claim costs.
4) Of particular note is the lower utilization rate for physical therapy and testing (lower visits per claim and lower percentage of claims receiving services. This may be attributable to the fact that the use of chiropractors is very low in Georgia.
“The Anatomy of Workers’ Compensation Medical Costs and Utilization: A Reference Book.” Workers Compensation Research Institute[33]
The evidence is incontrovertible that the chiropractic profession has been virtually eliminated from the WC program. For the entire year of 1999, chiropractors only accounted for 1.3% of the providers’ costs for back injuries. If this isn’t the profiling of a profession into obscurity, what is?
On a similar note, the American Chiropractic Association’s lawsuit against HCFA for cutting DCs out of the Medicare pie revealed that chiropractic’s utilization rate for Medicare managed care plans was only 1.08% in 1998, and for Medicare fee-for-service during the same period was a mere 4.15% to 4.42%; overall, chiropractic services among the American public is 6.5%.
As Dr. James Mertz, president of the ACA, said, “This report drives home the fact that the Medicare managed care patients are systematically being denied access to doctors of chiropractic…DCs are obviously being discriminated against in these plans…”
It appears that the same conclusion can be drawn from the WC stats here in Georgia. A case can be made that professional profiling and a general boycott of chiropractic care is on-going if these statistics are accurate.
Not only is this paltry amount for chiropractic services amazing, but so too is the high average cost of a case: $8,012, and the average settlement per case is $9,476. Accounting for all the WC expenses, the Total Payments All Cases was $432,638,094; almost a half-billion dollars alone on WC cases and this is down from the 1994 total of $779,327,793, which is to be applauded if these cuts were evenly across the board.[34]
If the WC Board desires to reduce this huge sum even more, I urge them to consider greater utilization of chiropractic care which has proven to be more clinical and cost-effective.[35]
5) Perverse Motivation by WC Insurance Companies & PI Attorneys
One huge problem facing the WC program is the “cost-plus” formula for insurance companies that basically allows them to charge more in premiums in order to cover their exposure. In this light, there is no motivation to reduce costs since insurance companies profit from their investments, not from their premiums.
This incentive has been termed a “perverse” motivation by economists in the field.[36] Consequently, the WC insurance carriers would prefer boycotting chiropractic care because it’s too cheap compared to surgery. In fact, they more they pay out, the more they can charge employers in higher premiums, so being the cheapest treatment is not an asset in this model. Indeed, employers are punished financially for this perverse motivation of the WC insurance companies wishing to keep costs high for their own profit.
On the other hand, one innovative IPA company in Highland Park, Illinois, Alternative Medical Inc, uses chiropractors as primary care physicians in the greater Chicago area and found huge reduction in costs for self-insured companies.
For example:
1) 80% reduction in hospital costs within 18 months
2) 85% reduction in out-patient procedures and surgeries
3) 56% reduction in pharmaceuticals
4) For patient satisfaction surveys, AMI achieved a 100% vs. a 60% for BCBS
5) For “thousands and thousands of member months” no back or neck surgeries have been performed on their patient population to date according to the president of AMI, Dr. Jim Zeckman.
Obviously in a self-insured environment where employers want to lessen their medical expenses, a program like AMI using preventative and conservative methods like chiropractic have proven to save time, money and lost work-days. In fact, where there is no incentive to pay more for costs in order to demand more in premiums to invest, the AMI approach has proven quite successful.
Perhaps this is one core problem with the current WC program in Georgia—this perverse motivation by the WC insurance companies. If profit is tied to expenses, obviously there is no motivation to lower costs. As many employers know, WC insurance is the most costly, most difficult to use, and when it is used, employers are punished with higher rates.
Another problem facing the WC program are the motives of PI attorneys who seek to increase medical costs in order to increase plaintiff’s settlements. Just as I’ve seen with auto accident cases, PI attorneys routinely refer most cases to the surgeons because a settlement starts at $25,000 rather than a few thousand for a chiropractic-resolved case. As long as WC insurance companies and PI attorneys are motivated to increase medical costs for their own profit, this perverse motivation will dictate which providers are chosen—the most expensive, of course.
6) Bias in the Workplace
Another problem voiced by many injured workers is the misinformation from claims adjusters and Safety/Personnel Directors who lie to them about chiropractic care. Whether they’re being told “chiropractic isn’t covered,” “you must see our MD gatekeeper for a referral to a DC,” or “you’ll be paralyzed if you go to a chiropractor,” these false statements simply fuel suspicion and unwarranted fear, and deny patients their rights to current proper standards of care.
I can’t tell you how many times injured-workers have told me that their Safety/Personnel Directors wouldn’t refer them to me because as they’re told, “I don’t believe in chiropractic.” Not only does this attitude smack of prejudice and ignorance, but it denies injured-workers their legal right to seek chiropractic care. All of these untrue negative comments may be lawsuits waiting to happen.
Another unethical ploy I’ve seen used by some biased Safety/Personnel Directors to intimidate workers into back surgery who desire chiropractic care is to threaten them with malingering if they refuse surgery. Some on-the-job-injured patients who are denied WC coverage for chiropractic care actually resort to paying for chiropractic care out-of-pocket, which is contrary to the basic idea of WC insurance covering on-the-job injuries.
Since few orthopedists rarely refer to DCs, injured workers are routinely forced into surgery that they didn’t want, didn’t need, but were intimidated into having surgery by unscrupulous, biased Safety/Personnel Directors.
I recommend that the WC Board mandate that every company post notices as to injured workers’ rights, including not only the panel of providers, but of the law that states they have the legal right to seek chiropractic care and a second opinion from a DC before surgery is scheduled.
7) The Role of Guidelines
The primary goal of guidelines is to improve standards of care by bringing the most up-to-date knowledge to clinical practice in a form that is easy to use. The biggest challenge is to have health professionals understand and adopt guidelines—to change their settled habits of clinical practice to be consistent with current knowledge.
A major education campaign aimed at the entire range of health care professionals as well as a major public education campaign through the mass media will be necessary if these recommendations in favor of early conservative, non-invasive activity are to be heard and accepted.
Obviously the expert opinion of researchers from the US, UK, Denmark, among others, believe a lot of money could be saved by employers and payers, and many lost work-days and suffering/disability could be avoided by workers if chiropractic care were the first choice of care as per their guidelines.
At the December 8, 1994 press conference introducing the AHCPR guideline on acute low back pain in adults, Philip R. Lee, MD, assistant secretary for Health and Human Services and head of the Public Heath Services, “These guidelines could save Americans considerable anguish, time and much money now spent on unneeded and unproved medical care.”
Also at the same press conference, Clifton R. Gaus, Sc.D., administrator of AHCPR, also mentioned in the news release that “…a preliminary cost analysis of these guidelines suggests the nation could save as much as a third of the medical expense of treating this condition without any loss of quality of care.”
If the WC Board hopes to improve its program with improved clinical and cost-effectiveness, it must move toward evidenced-based medicine, which means doing what is supported by research rather than what’s most profitable to the status quo.
According to the comprehensive Canadian meta-analysis on back pain by Pran Manga, Ph.D, “The Effectiveness and Cost-Effectiveness of Chiropractic Management of Low-Back Pain,” this evidence-based study concluded:
“In our view, the constellation of the evidence shows:
1) the effectiveness and cost-effectiveness of chiropractic management of low-back pain.
2) the untested, questionable or harmful nature of many current medical therapies.
3) the economic efficiency of chiropractic care for low-back pain compared with medical care.
4) the safety of chiropractic care.
5) the higher satisfaction levels expressed by patients of chiropractors.
Dr. Manga was very realistic about the turf warfare in the healthcare business:
“There should be a shift in policy now to encourage the utilization of chiropractic services for the management of LBP, given the impressive body of evidence on the effectiveness and comparative cost-effectiveness of these services, and on the high levels of patient satisfaction.
“The shift in utilization from physician to chiropractic care should lead to significant savings in healthcare expenditures judging from evidence in the Canada, the US, the UK and Australia, and even larger savings if a more comprehensive view of the economic costs of low back pain is taken.
“Unnecessary or failed surgery is not only wasteful and costly but, ipso factor, low quality medical care. The opportunity for consultations, second opinions and wider treatment options are significant advantages we foresee from this initiative which has been employed with success in a clinical research setting at the University Hospital, Saskatoon.
“A prominent medical organization, the North American Spine Society, has recently concluded that spinal manipulation, and specifically chiropractic adjustment, is an acceptable and effective treatment for most patients with lumbosacral disorders. This review, when coupled with more thorough analysis by prestigious institutions such as RAND Corporation, adds measurably to the growing credence in spinal manipulation as a therapy of choice for most low back pain.”
“However, the desired change in the healthcare delivery system will not occur by itself, by accommodation between the professions, or by actions on the part of Workers’ Compensation boards or the private sector generally. The government will have to instigate the reform and monitor the progress of the desired changes called for by our overall conclusion.” [37]
8) Back Pain Guidelines from Denmark
Through its National Board of Health, Denmark has recently published clinical guidelines for the prevention and management of low back pain.[38] These guidelines have been received as authoritative in Denmark, and are already being acted upon.
“There is so much new demand for chiropractors in hospital back clinics and interdisciplinary primary care centers that the chiropractic profession cannot meet it,” said Dr. Henrik Laugesen, DCA President.
The Danish study found the “vast majority of back pain—over 90% of cases—arises from functional pathology (ie mechanical problems of the joints and muscles) rather than structural pathology (degenerative or herniated discs, bone spurs).
Each treatment method is assigned to one of three chapters which respectively list treatments as:
a) Generally Recommended—manual therapy; back school/ergonomics; pain relieving medication; exercise therapy to McKenzie; exercise therapy/fitness.
b) Recommended in Certain Condition—injections in muscles/trigger points/ligaments/joints; epidural injections; acupuncture; massage and heat/ice therapy; back surgeries; bed rest; TENS.
c) Cannot be Recommended—corsets, traction, ultrasound/laser/short wave therapy.
Manual therapy–spinal manipulative therapy, mobilization, manual traction, myofascial release and muscle energy techniques are all included within the generally recommended treatment ‘manual therapy’ which is defined as “all procedures where the health professional uses his/her hands in order to influence the joint complex as well as surrounding tissues. Treatment is given in order to relieve pain and improve function.”
Manual therapy is recommended:
a) For patients with acute pain and functional limitations of more than 2 or 3 days duration.
b) For acute exacerbations of recurrent or chronic low-back pain and functional limitation.
c) As one element of a broader strategy for chronic low-back pain problems.
d) As an element of a conservative treatment regime for many patients with nerve root irritation/disc problems.
e) Contraindications given for manual therapy are cancer, inflammation, infection and serious and/or progressive nerve root irritation.
f) Strict criteria are given for all forms of surgery. Disc surgery should not usually be performed “before conservative therapy has been attempted for 4-6 weeks.” Stabilizing back surgeries, because of limited evidence of effectiveness, high cost and complications, “can only be recommended in particularly well-chosen cases” and should be performed at a few specialist centers only.
9) A Chiropractic Proposal to Save Money and Lost Work Days
My proposal to the WC Board is to choose the US, UK, Canadian or Danish guidelines for all WC providers to follow. Select qualified chiropractic spinal rehab facilities across the state to send injured workers with neck or back problems. Of course, not all DCs have the proper equipment, training or staff to implement these extensive guidelines, just as all PTs and MDs do not qualify for these cases. I would recommend the use of Guardian Care, a PPO of certified DCs across the state with at least 5 years of experience or those DCs who are certified in rehab care by the Chiropractic Rehabilitative Association.
No one aware of the research and facts about LBP treatments will argue that spinal manipulative therapy doesn’t work. That is an out-dated false opinion based on bias than fact. Actually, the most knowledgeable researchers question the validity of most medical methods, not chiropractic care. As Dr. Manga of the Ontario Ministry of Health mentioned in his report, “There is, for example, a thought-provoking claim from an eminent neurosurgeon in the US that approximately 90% of the 250,000 back surgeries performed annually in that country could be avoided (Burton et al., 1992).”
Even if chiropractic care were the same cost with the same outcomes as surgery, patients should still be entitled to a non-invasive alternative to surgery if that’s their preference. Regardless of choice, the institutional medical approach to back pain is not only costly, but delays proper treatment for many injured workers.
According to Dr. Manga’s study:
“For patients to go to the wrong or sub-optimal caregivers first only to have to go to the more optimal caregiver later, clearly implies unnecessary costs of care to insurers and patients and poorer health outcomes…Currently an overwhelming majority of patients with NMS conditions and injuries visit medical doctors first. A staggering 81% of patients of chiropractors have had their back pain or other NMS disorders for more than 6 months and, typically, would have had extensive medical and/or physiotherapy care up to the time they decided to see a chiropractor. This suggests both an enormous amount of wasted health care expenditure and worsening health of the patients.[39]
“The central argument that leads us to this conclusion is that chiropractors are highly cost-effective alternative providers of care for neuromusculoskeletal conditons…Needless to say, the cost-effective matching of needs and caregivers should be based on evidence and not merely on tradition and the unquestioned acceptance of the status quo…There is, thus, much evidence showing that greater chiropractic coverage under private or public insurance generates significant savings in health care costs…The savings for patients for whom surgery was avoided can run over $18,000 on average!…Chiropractic should be a frontline service rather than the default (i.e., when all else fails) system of care it seems to be for many patients.”[40]
What has this profiling of chiropractic to the margins of Georgia’s WC program led to? A huge waste of money, the abuse of patients with ineffective back surgeries, and a lack of informed consent and their freedom of choice in regards to the best form of LBP care. There is no good reason why chiropractic care should be limited in any manner if the WC Board is interested in eliminating waste, abuse of the system by unscrupulous surgeons, and giving patients the best care possible.
Inasmuch as a case can easily be made that for the majority of mechanical low back, neck and wrist injuries, manipulation is the most effective treatment, I would like to challenge the WC Board to implement a carve-out study proposal similar to what transpired in south Florida at an HMO that utilized chiropractic care.
The Miami-based HMO, AV-MED, found that 86% of 100 patients medically unresponsive were treated by a chiropractor saving the HMO over $250,000. [41]
Another study done in Florida by Dr. S. Wolk, Ph.D., in a review[42] of 10,000 cases from 1985-87 showed that:
1) disability was 48.7% shorter under chiropractic care.
2) 51% of medical patients were hospitalized compared to only 20% of chiropractic patients.
3) average total cost of care was 84% higher for medical group; $1,204 (chiropractic) vs. $2,213 (medical)
I recommend the use the AHCPR federal guideline to screen all patients, then to treat according to the guideline’s algorithm. Evaluate the results to see if they match those obtained in Florida. Let’s have the evidence decide which type of treatment is best rather than the bias and medical prejudices that have prevailed for too long.
I daresay the chiropractic management of back problems would save the WC program millions of dollars annually. If the AHCPR is correct in its statement that only one in 100 back surgeries is helpful, the potential savings is huge. Is the WC Board ready to implement a chiropractic program that could reduce costs anywhere from 50-90% of the present costs for LBP? This is the challenge we chiropractors propose.
10) Failed Back Surgery Syndrome: Throwin’ Good Money After Bad
“71% OF WORKERS’ COMPENSATION PATIENTS UNDERGOING FIRST LUMBAR SURGERY DO NOT RETURN TO WORK; 95% OF MULTIPLE SURGERIES DID NOT”
This study, “Late postoperative results in 1000 work related lumbar spine conditions,” was reported in Surgical Neurology 54(2) in August, 2000 by Berger. It was done due to the poor results that are so often reported following operation of the lumbar spine in Workers’ Compensation cases. One thousand patients, 600 of who had one lumbar spine surgery and 400 with multiple surgeries were followed post-surgically for 51 and 38 months, respectively.
71% of single operated and 95% of multiply operated patients did not return to work more than 4 years after the surgery, even though no neurological deficits that precluded employment were present. The chronic postoperative pain was cited as the reason for failure to return to work. The role of psychosocial factors versus the role of chronic pain must be determined to prevent this failure of return to work.
As I look at this finding, I think of my own practice and note that the number of patients failing to return to work is almost unheard of. The occasional case that does not return to work is usually preceded to seeing me by having visited medical doctors, therapists, psychologists, and many specialists. By the time they do get to me they are so depressed and angry that they need much encouragement to return to normal activities of daily living. They are medicated, injected, operated on, and mad. That is the reason that I always start patients on basic exercises of knee chest, abdominal stabilization exercises, and walking when they are first seen.
At times I feel like “all the King’s men trying to put Humpty Dumpty back together again.” My heart goes out for those victims of unnecessary and ineffective back surgery considering that most are misdiagnosed, mistreated, misinformed, and never told that chiropractic care is an alternative (lack of informed consent).
Encouragement and awareness of help to get well are vital in treating chronic low back pain. Naturally, some cases require interdisciplinary care with counseling, pain control, etc., but the main ingredient is chiropractic adjusting; in my case that is distraction adjustment procedures. There is a need for chiropractic care to be plugged into the equation of treating these chronic low back pain sufferers. Since joint dysfunction constitutes over 70% of these mechanical back pain disorders according the recent article by Richard Deyo in the New England Journal of Medicine, chiropractic adjustments are essential if the patient is to regain his good spinal health.
In an article titled: PATIENTS WHO SUFFER CHRONIC PAIN DISSATISFIED WITH TREATMENT:
Patients with chronic pain are dissatisfied with the efficacy of their prescription and over the counter pain control medications. 66% of 1000 people surveyed said over the counter drugs were not completely or very effective and 52% of those relying on prescription drugs said they were not completely or very effective.
Many patients had pain for years with 62% experiencing pain for at least 5 years. Often it took along time to control the pain, and 43% of patients suffered for a year or more before they felt their pain was under control, and for 21% it took 5 years or longer. 78% of them are willing to try new treatments and 43% would spend more on a treatment if they knew it would work. These statistics are from a national survey commissioned by Partners Against Pain, an educational program sponsored by Purdue Pharma.
Physician satisfaction relates to pain relief with care. Unhappy patients find that 62% of them cite unsuccessful treatment as the reason. They feel their physician has not helped them or is not doing enough to heal them. Extensive effort is put forth by patients to receive pain relief; on average they have seen 3 physicians for their pain and have taken 3.7 different kinds of prescriptions for pain. They travel great distances to seek relief. 80% of pain patients feel their pain is a normal part of their medical condition and 33% feel they can’t function as normal people and sometimes feel so bad they want to die.
The aspects of daily living interfered with by pain are:
- 56% have interference with sleep
- 51% have mood affect
- 30% have driving affected
- 28% have sexual relations problems
- 7% inability to feed themselves
Pain is related to the following body parts:
- Skeletal problems – 48% and include back pain, knees, neck, shoulder/arm, ankle/foot, joints, bones, hips and bursitis
- Arthritis – 28%
- Headaches – 16%
- Nerve problems – 19%
- Surgical/postoperative – 4%
- Traumatic injury – 2%
Pain costs more than 100 billion dollars a year to treat in the U.S. according to the National Institutes of Health. Forty percent of patients feel uncomfortable discussing their pain with family members and 37% say pain is isolating.
One of the largest costs of any WC program is the permanently disabled patient suffering from failed back surgery syndrome. In many cases, these patients have had not one but multiple surgeries before they are given a morphine pump, told to go home and live on disability for the rest of their lives.
Researchers have noted this epidemic of failed back surgery with very poignant comments. Dr. Gordon Waddell mentions that the high disability rate is actually enhanced by medical methods:
“Sadly, we must conclude that much low back disability is iatrogenic [doctor-caused]…It [back surgery] has been accused of leaving more tragic human wreckage in its wake than any other operation in history…There is now considerable evidence that manipulation can be an effective method of providing symptomatic relief for some patients with acute LBP.”[43]
The AHCPR guideline also mentions the low success rate of back surgery and fusion in particular.
“Moreover, surgery increases the chance of future procedures with higher complication rates.”[44]
“There appears to be no good evidence from controlled trails that spinal fusion alone is effective for treatment of any type of acute low back problems in the absence of spinal fracture or dislocations…Moreover, there is no good evidence that patients who undergo fusion will return to their prior functional level.”[45]
Noted medical author, Dr. Ruth Jackson, formerly chief of orthopedic surgery and instructor at Baylor University College of Medicine in Dallas, wrote the mainstay of textbooks on neck problems summarized the true indications for fusion:
“When, then, should fusion be done? Certain fracture-dislocations with marked instability may need fusion. Marked ligamentous instability with spinal cord irritation, or if there is danger of cord involvement, may indicate the necessity for fusion…Surgery should be avoided unless there are absolute and definite indications for it, otherwise the results from operative procedures will be disappointing and the symptoms may be worse than they were before surgery was done.”[46]
Another study conducted in 1994 by Drs. D.C. Cherkin, R.A. Deyo, J.D. Loeser, T. Bush, and G. Waddell compared international rates of back surgeries and found the startling fact that American surgeons are unusually excessive.
“The rate of back surgery in the United States was at least 40% higher than any other country and was more than five-times those in England and Scotland. Back surgery rates increased almost linearly with the per capita supply of orthopedic and neurosurgeons in that country.”[47]
The AHCPR panel also found that 5% of low back patients accounts for 60% of the costs, principally these victims of unnecessary and ineffective back surgery. Factoring in the permanent disability costs for patients of failed back surgery syndrome, there’s a large possibility that SMT could save Georgia’s WC program millions of dollars.
For example, in 1999, the WC program incurred 119,039 lost work days, $13,169,569 in indemnity costs, and $11,453,569 in medical costs for 2898 cases of back injuries. If chiropractic care could save just 50% of these cases, that would save millions of dollars for the overall WC program. In theory, I daresay up to 90% of these cases and costs could be reduced with SMT.
I urge the WC Board to conduct a study to determine the number of failed back surgery victims and their costs. I think this study may find, as the ACHPR panel found, that a small percentage of failed back surgeries have incurred much of these monies.
But the problem remains: How do you handle these victims of failed back surgeries? Obviously more surgeries is equivalent to throwing good money in after bad. I suggest the Board develop a program of spinal rehab consisting of SMT along with active spinal rehab consisting of continuous passive motion to restore joint motion and spinal strengthening to restore tone and strength. Without such a rehab program, these patients have no hope of improvement, they will continue to decondition and degenerate, leading to more costs and suffering.
Again, every panel of inquiry on back disorders concluded that spinal fusion is inappropriate and ineffective for non-traumatic cases and standard physical therapy consisting of passive modalities do nothing to correct the underlying problem of joint dysfunction.
If there is any hope for these victims, it rests with the actual rehabilitation of their weak backs, just as you would do for them if they had suffered from a football knee injury—you must restore alignment of the joint, restore full flexibility of the joint, then strengthen the muscles around the joint. This translates into SMT and spinal exercises.
Only then will the affected joint be stabilized and, as you can extrapolate, spinal surgery accomplishes none of these factors. In effect, fusion simply fuses vertebrae in the misaligned position, consequently, the primary source of back pain stemming from the joint dysfunction is not even addressed leading to continued pain, more surgeries, and in reality, throwin’ good money in after bad.
11) Informed Consent—Quiz Your Doctor
In the September 19, 2000 edition of USA Today, an article titled, “Patients need to cut out total trust in physicians,” appeared and suggested that patients ask questions before major surgery. Of the types of surgery with the widest variation, back surgery ranked number six. According to Medicare statistics, Macon ranked first in back surgeries in Georgia. These statistics came from the Dartmouth Atlas of Health Care.
Since many WC patients are usually directed into back surgery without informed consent being obtained, I suggest the WC Board might follow the advice given in this article. Here is a list of questions they suggest using as Informed Consent:
1) What are the risks and benefits of all the alternatives to the surgery, including doing nothing or delaying the procedure?
2) What is the second opinion of a doctor unconnected with your, one who doesn’t share any financial or local ties to your physician?
3) How often has your surgeon performed this surgery? How often do complications occur, what are they, and what are their effects?
4) Do any medical disagreements exist over the procedure or the diagnostic tests used to indicate this course of action?
5) What are the chances the surgery will have to be repeated later? If so, how soon?
6) Can a friend accompany me when we discuss all the alternatives? Can I tape record the discussion?
7) What are the guidelines recommended for my case? (A written explanation of the AHCPR guideline would be appropriate)
Instead of informed consent, most patients are given “uninformed consent” according to the USA Today article. “It is a situation born of inadequate medical science, opinion parading as knowledge, over-reliance on inadequately verified diagnostic tools and basic inequities in the health care system.”[48]
In the situation of chiropractic profiling, the same can easily be said. Consider the “inadequate medical science” when MRI research and the AHCPR guideline state that disc abnormalities are not the cause of most back problems; “opinion parading as knowledge” when surgeons tell patients that “chiropractic will paralyze them” when, in fact, the facts prove spinal manipulation is far, far safer than surgery; “over-reliance on inadequately verified diagnostic tools” is seen with the over-use of MRI that never show joint dysfunction, instead focusing solely on disc pathologies which have little to do with back pain according to MRI researchers; and “basic inequities in the health care system” when chiropractic incurs less than 1% of the WC expenses last year despite the fact that according to OSHA neck, wrist and back MSDs constitute the largest group of on-the-job injuries.
According to a recent case (Jean Matthies v. Edward D. Mastromonaco, DO) argued before the Supreme Court of New Jersey on February 19, 1999, a unanimous decision was handed down on July 8 of the same year when a doctor was sued for lack of informed consent.[49] This decision extended the rights of the patient with regards to alternative medical treatment in general:
1) “In turn, the doctor has the duty to evaluate the relevant information and disclose all courses of treatment that are medically reasonable under the circumstances. It is for the patient to make the ultimate decision regarding treatment based on the doctor’s recommendations. Informed consent applies to invasive and noninvasive procedures.
2) “To ensure informed consent, the physician must inform patients of medically reasonable alternatives and their attendant probable risks and outcomes. Physicians do not adequately discharge that duty by disclosing only the treatment alternatives that they recommend.
3) “A physician should discuss the medically reasonable course of treatment, including non-treatment.
4) “Like the deviation from the standard of care, the doctor’s failure to obtain informed consent is a form of medical negligence. Recognition of a separate duty emphasizes the doctor’s obligation to inform, as well as treat, the patient.”
This decision places a lot of pressure upon anyone who is rendering medical care. By positioning informed consent as an indicator for “standard of care,” it demands a far more acute level of awareness and appreciation of other healthcare options than previously. Ignoring such information in clinical practice becomes virtually indefensible, if not tantamount to outright malpractice. This decision also is a major vindication for the rights of patients to have all the relevant information available to them to make important decisions about the care of their own bodies.
Here in Georgia it’s been my professional experience with patients suffering from failed back surgery that surgeons are not obtaining from patients true informed consent. Patients are not being told of their options and alternatives, nor are they told the honest iatrogenic rates for surgery or manipulation. Instead, many are told that spinal manipulation will “paralyze you” when, in fact, SMT causes problems in only 1-2 cases per million compared to 15,600 strokes/paralysis per million for surgical cases. Mortality rates for SMT are 3 in 10 million cases, whereas deaths from neck surgery are 6,900 per one million.[50] Indeed, who’s hurting who?
Unfortunately, this type of voodoo diagnosis by unethical surgeons is enough to frighten unsuspecting patients into a back surgery they may not have needed. Legally, this does not constitute “informed consent” or meet the present “standards of care” by any means, yet it is done routinely by some surgeons.
I recommend a written informed consent sheet developed by the WC Board be developed and used in every case. Since one goal of the WC Board is to avoid costly lawsuits, by adhering to a written informed consent form many problems such as seen in the Matthies v. Mastromonaco case could be avoided. The virtual railroading of injured patients into back surgery without ethical, legal informed consent is a major lawsuit just waiting to happen. And when it does, without a written informed consent form available, this oversight will become a costly nightmare.
12) Recommendations:
It’s painfully obvious that the WC program in Georgia has a paradox: On one hand the WC program wants to reduce costs, on the other hand, it has ignored the best cost-saving method—chiropractic care for the majority of low back, neck and wrist cases, the leading work-related injuries according to OSHA.
The proof is clear that the current WC system is awash with:
1) discrimination against chiropractors,
2) exploitation of injured workers without informed consent nor given a freedom of choice of the proper standard of care treatments,
3) a refusal to follow established guidelines,
4) a lack of ethics by insurance adjusters, personnel directors and gatekeeper MDs who mislead patients about the safety and availability of chiropractic care within WC,
5) and a waste of money by employers who pay for the indulgences of unnecessary back surgeries by medical providers.
Obviously every issue that the USA Today article criticized is happening within Georgia’s WC program. Does this Advisory Council have the integrity to confront these issues, or will we see a cover-up to maintain the status quo and to continue the boycott of chiropractic care? Is the Board culpable for these mistakes, over-sights and the marginalization of chiropractic care that leads to unnecessary costs, waste, and abuse of patients? Indeed, who is at fault for this obvious negligence?
If this Council is ready to improve the inequities within the WC program, if it is ready to save employers millions of dollars, save patients from ineffective and unnecessary surgeries, and give patients a choice in their own healthcare matters, I would like to make some recommendations.
1) Review thoroughly the evidence-based cost and clinical-effectiveness of each type of treatment as the Canadian, US, UK, and Danish governments have already done conclusively.
2) Allow direct access to full-scope chiropractic care without MD gatekeepers.
3) Establish a realistic guideline or follow the AHCPR guideline on LBP which recommends conservative care first and surgery last. This guideline will also act to eliminate over-treatment by DCs and PTs, the high costs from ineffective back surgeries and unnecessary routine tests like MRI exams.
4) Post notices in every Safety/Personnel Director’s office that injured workers have the legal right to see a doctor of chiropractic to end their bias and discrimination.
5) Establish punishment for Safety/Personnel Directors or WC insurance adjusters who lie about the safety of chiropractic care or deny access without cause.
6) Provide mandatory sensitivity classes to Safety/Personnel Directors and insurance administrators on the facts concerning LBP treatments to end professional profiling.
7) Mandate a true second opinion from a DC before any back surgery is done to end waste and unnecessary surgeries/tests.
8) Establish sanctions for any surgeon who misleads patients about their condition, fails to do informed consent with patients as to alternatives, or lies about the safety of chiropractic care.
9) Maintain statistics on clinical outcomes done by each WC provider to determine the clinical and cost-effectiveness of each treatment.
10) Full informed consent must be given and signed by each patient citing the recommended procedures, side-effects of treatment, and rates of injury. A standard form issued by the SBWC which is read and signed by every patient would be appropriate.
11) Place DCs on every Panel of Physicians to give injured workers a freedom of choice. The code now states that the “traditional posted panel” must include one “minority” physician. While this generally includes racial minorities, I suggest it be extended to include minority practitioners such as chiropractors. “The Board reserves the right to allow exceptions when warranted” may be applied to allow DCs on this panel.
12) As well, the “conformed panel of physicians” which “shall include a minimum of ten physicians or professional associations and the following additional healthcare services: general surgeons and chiropractors.” I suggest this conformed panel be implemented immediately and include DCs.
13) Allow the GCA Peer Review to review any disputed chiropractic claims and to admonish or remove unethical chiropractic practitioners to prevent waste and abuse.
14) An annual follow-up study be done to determine the savings involved from the full utilization of chiropractic care.
Conclusion
I hope this report will provide the WC Board with accurate information in order to make an informed decision to improve this program. The need is clear, the evidence is incontrovertible, and the waste of money on ineffective back surgeries and distributive injustice to DCs are obvious. If the Board wants to improve the outcomes of injured workers, lessen the medical costs, and decrease the financial cost to employers, the choice for parity and access to chiropractic care will accomplish this goal.
[1] S. Bigos, et al., “Acute Low Back Problems in Adults, Clinical Practice Guideline No. 14,” U.S. Public Health Service, U.S. Dept. of Health and Human Services, AHCPR Pub. No. 95-0642, Rockville, MD: Dec. 1994.
[2] Manga, P and Angus, D. “Enhanced chiropractic coverage under OHIP as a means of reducing health care costs, attaining better health outcomes and achieving equitable access to select health services.” Working paper, University of Ottawa, 98-02.
[3] Eccleston, S. et al. “The Anatomy of Workers’ Compensation Medical Costs and Utilization: A Reference Book.” Workers Compensation Research Institute, Cambridge, Mass. June, 2000
[4] Manga, P. ibid.
[5] S. Bigos, et al., “Acute Low Back Problems in Adults, Clinical Practice Guideline No. 14,” U.S. Public Health Service, U.S. Dept. of Health and Human Services, AHCPR Pub. No. 95-0642, Rockville, MD: Dec. 1994.
[6] Bernard, B., Fine, L., eds. [Bernard et al, 1997]. Musculoskeletal Disorders and Workplace Factors. Cincinnati, OH: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control, National Institute for Occupational Safety and Health. DHHS (NIOSH) Publication #97-141. Ex. 26-1
[7] Shekelle, P. et al. RAND Corp Report, “The appropriateness of spinal manipulation for low-back pain,” Santa Monica, Calif. 1992.
[8] S. Bigos, et al., “Acute Low Back Problems in Adults, Clinical Practice Guideline No. 14,” U.S. Public Health Service, U.S. Dept. of Health and Human Services, AHCPR Pub. No. 95-0642, Rockville, MD: Dec. 1994.
[9] S. Bigos, et al., “Acute Low Back Problems in Adults, Clinical Practice Guideline No. 14,” U.S. Public Health Service, U.S. Dept. of Health and Human Services, AHCPR Pub. No. 95-0642, Rockville, MD: Dec. 1994.
[10] S. Bigos, et al., “Acute Low Back Problems in Adults, Clinical Practice Guideline No. 14,” U.S. Public Health Service, U.S. Dept. of Health and Human Services, AHCPR Pub. No. 95-0642, Rockville, MD: Dec. 1994.
[11] Her Majesty’s Stationery Office in London in its Report of a Clinical Standards Advisory Group Committee on Back Pain, 1994
[12] Waddell G. The Back Pain Revolution. Churchill Livingston, Edinburgh, 1998.
[13] S.D. Boden et al., “Abnormal Magnetic-Resonance Scans of the Lumbar Spine in Asymptomatic Subjects,” J. Bone Joint Surgery (AM) 72(3):403-8 (1990).
[14] Finneson BF. A lumbar disc surgery predictive score card: a retrospecive evaluation,” Spine (1979): 141-144.
[15] Kirkaldy-Willis WH and D. Cassidy, Can. Fam. Phys. 31 (1985): 535-40.
[16] Bogduk N. Clinical anatomy of the lumbar spine, pp. 170.
[17] Mooney V, Spine 12(6):754-59 (1987).
[18] Webser BS, Snook SH. The cost of 1989 workers’ compensation low back claims. Spine 19(10):1111-1116, 1994.
[19] M. Mushinski, “Average Hospital Charges for Medical and Surgical Treatment of Back Problems: United States, 1993,” Statistical Bulletin, Metropolitan Life Insurance Co., Health and Safety Education Division, Medical Dept., April-June 1995.
[20] P. Shekelle, et al, “The Appropriateness of Spinal Manipulation for Low Back Pain.” RAND Corporation Report, Santa Monica, Calif., 1992.
[21] Cailliet R. Therapeutic Approaches to Low Back Pain. Am J Clin Chiro 1999;
9(4): 1&5.
[22] Mendelsohn R. Confessions of a Medical Heretic, 1978.
[23] Seaman, D. Joint complex dysfunction, a novel term to replace subluxation/subluxation complex. Etiological and treatment considerations. J. Manip Physiol Ther 1997, 20:634-44.
[24] Jensen, M.C., et al., “Magnetic resonance imaging of the lumbar spine in people without back pain,” The New England Journal of Medicine, 3313(2):60-73 (1994).
[25] S. Bigos, et al., “Acute Low Back Problems in Adults, Clinical Practice Guideline No. 14,” U.S. Public Health Service, U.S. Dept. of Health and Human Services, AHCPR Pub. No. 95-0642, Rockville, MD: Dec. 1994.
[26] S. Bigos, et al., “Acute Low Back Problems in Adults, Clinical Practice Guideline No. 14,” U.S. Public Health Service, U.S. Dept. of Health and Human Services, AHCPR Pub. No. 95-0642, Rockville, MD: Dec. 1994.
[27] Deyo, RA. Low -back pain., Scientific American, pp. 49-53, August 1998.
[28] Deyo RA, Psaty BM, et al. The Messenger under Attack–Intimidation of Researchers by Special-Interest Groups, NEJM, vol. 336, No. 16, pp. 1176-79, April 17, 1997.
[29] Manga, P and Angus, D. “Enhanced chiropractic coverage under OHIP as a means of reducing health care costs, attaining better health outcomes and achieving equitable access to select health services.” Working paper, University of Ottawa, 98-02.
[30] Eccleston, S. et al. “The Anatomy of Workers’ Compensation Medical Costs and Utilization: A Reference Book.” Workers Compensation Research Institute, Cambridge, Mass. June, 2000
[31] Mushinski, M. ibid.
[32] Eccleston, S. et al. “The Anatomy of Workers’ Compensation Medical Costs and Utilization: A Reference Book.” Workers Compensation Research Institute, Cambridge, Mass. June, 2000.
[33] Eccleston, S. et al. “The Anatomy of Workers’ Compensation Medical Costs and Utilization: A Reference Book.” Workers Compensation Research Institute, Cambridge, Mass. June, 2000.
[34] Georgia State Board of Workers’ Compensation web page. (www.ganet.org/sbwc/about/)
[35] Manga, P. ibid.
[36] Bezold, C. “The future of chiropractic: Optimizing Health Gains” Institute for Alternative Futures. July 1998.
[37] Manga Pran, PhD et al. “The Effectiveness and Cost-Effectiveness of chiropractic Management of Lob-Back Pain, “ Ontario Ministry of Health, 1993
[38] Manniche C et al. Low-back pain: Frequency, management and prevention from an HDA perspective. Danish Health Technology Assessment 1999: 1(1).
[39] Manga, P and Angus, D. “Enhanced chiropractic coverage under OHIP as a means of reducing health care costs, attaining better health outcomes and achieving equitable access to select health services.” Working paper, University of Ottawa, 98-02.
[40] Manga, P ibid.
[41] Silverman M, “Study of the first 100 patients referred to the Silverman Chiropractic Center by AV-MED,” The Chiropractic Report, vol. 2, no. 2, Jan. 1988.
[42] Wolk, S., “Chiropractic vs. medical care: A cost analysis of disability and treatment for back-related workers’ compensation cases.” Foundation for Chiropractic Education and Research, Arlington, VA. Sept. 1988.
[43] Waddell G. and OB Allan, “A historical perspective on low back pain and disability, “Acta Orthop Scand 60 (suppl 234), 1989,.
[44] S. Bigos, et al., “Acute Low Back Problems in Adults, Clinical Practice Guideline No. 14,” U.S. Public Health Service, U.S. Dept. of Health and Human Services, AHCPR Pub. No. 95-0642, Rockville, MD: Dec. 1994.
[45] S. Bigos, et al., “Acute Low Back Problems in Adults, Clinical Practice Guideline No. 14,” U.S. Public Health Service, U.S. Dept. of Health and Human Services, AHCPR Pub. No. 95-0642, Rockville, MD: Dec. 1994.
[46] Jackson, R. “The Cervical Syndrome.”
[47] Cherkin, DC et al., “International comparison of back surgery rates, “ Spine 19 (11): 1201-1206 (1994).
[48] USA Today, Sept. 19, 2000, an article titled, “Patients need to cut out total trust in physicians.”
[49] Jean Matthies v. Edward D. Mastromonaco, DO. Supremem Court of New Jeersey [A-9-98], Pollock J. Judgement dated July 8, 1999.
[50] P. Shekelle, et al, “The Appropriateness of Spinal Manipulation for Low Back Pain.” RAND Corporation Report, Santa Monica, Calif., 1992.