Fake News in Medicare
The recent revelation about “fake news” in the media, Facebook Mounts Effort to Limit Tide of Fake News, may come as a shock to many unsuspecting Americans, but not to chiropractors who have been victimized by old fashion medical propaganda and yellow journalism certainly since the organization of the Committee on Quackery in the 1960s, long before the advent of the internet and long before propaganda was called fake news.
Most recently we’ve seen two examples of fake news go viral with the pediatric chiropractic witch hunt Down Under and in the US we’ve seen the Katie May accident. In both cases, our image was impugned by the slanted, bias news reporting without any significant feedback from our leadership or by “fair and balanced” reporters giving our side to these issues. In both cases, we were slam-dunked!
Once again we witness another assault on chiropractic, “Medicare Paid Chiropractors Bone-Chilling Millions for Bogus Billings,” that went viral across this country when the OIG declared chiropractors defrauded Medicare by $359 million.
Let’s put this into comparison. Since 2010, federal authorities operating as part of the “Fraud Takedown” initiative have arrested and charged roughly 1,200 people allegedly complicit in defrauding the Medicare and Medicaid programs of more than $3.5 billion.[1]
However, the alleged $359 million chiropractic fraud compared to $3.5 billion equates to 0.1%, but this goes unmentioned by the media. Plus this $3.5 billion failed to make the same grade of national attention as did the chiropractic fraud and it certainly did not go viral.
Wonder why?
The following article came from Mark Schoene, editor of The BackLetter (Vol. 32, No. 1, January 2017). Mr. Schoene is undoubtedly among the most astute journalist concerning the spine profession who raised some important objections to the attack on chiropractic.

Curious Chiro-Hostility
A US government agency has leveled dramatic but inaccurate accusations against American chiropractors—accusing them of overcharging the US government and its Medicare program by $359 million in 2013 alone. An investigation by the Office of the US Inspector General concluded that 82% of the chiropractic treatment billed to the US government was “medically unnecessary” and should have been disallowed.
This report led to some terrible publicity for chiropractic:
- “Medicare Paid Chiropractors Bone-Chilling Millions for Bogus Billings,” according to a headline in the Fiscal Times.
- “Medicare overpaid for most chiropractic services. Will patients have to repay?,” according to the Washington Post.
- “Medicare Wasted $359 Million on Superfluous Chiropractic Treatments,” trumpeted The Daily Caller.
Misinterpretation of Claim Requirements and the Scientific Evidence?
However, on further reading this report seems curiously off-base. For instance, it appeared to misinterpret the evidence—and documentation requirements—on extended chiropractic treatment (i.e. treatment lasting more than 90 days).
The report repeatedly implied that treatment for acute or chronic pain that lasted more than 90 days may be “medically unnecessary” and would qualify as “maintenance therapy,” which is not covered under Medicare policies.
Yet, extended treatment for appropriate indications is fully allowed under Medicare regulations—even if the Inspector General believes otherwise. Chronic pain often waxes and wanes for months and years—as do episodes of care.
The report from the Inspector General condemned dozens of episodes of care for not documenting the medical necessity of those claims. Yet, it did not provide concrete examples of the errors in documentation. Is the Inspector General trying to improve documentation or simply condemn chiropractic care? Did the failures in claims documentation simply stem from poorly written administrative claim forms, or complex documentation requirements—or something more sinister, as the Inspector General alleges? It is impossible to tell from reading the report.
And the report was sloppy. For instance, any claim for chiropractic services under Medicare has to be coded with an “AT” designation—AT standing for “Active Treatment.” This would be active treatment intended to improve patients’ symptoms and functional status. This designation can be applied to the treatment of acute or chronic pain.
According to Medicare policies, if a claim is not accompanied by an AT designation, it is automatically classified as “maintenance therapy”—which is not eligible for Medicare payment. But the Inspector General’s report erroneously defined the AT designation as “Acute Treatment,” which is misleading.
Cross-Section of Medicare Claims
The report from the Inspector General looked at a representative cross-section of Global Spine Care practice claims submitted to the Centers for Medicare & Medicaid Services (CMS), including 105 services.
Here is the segment of that report, which condemned chiropractic treatment lasting more than 90 days:
The chiropractors submitted claims for all 105 services with the AT modifier and initial treatment date, indicating that the services were for active/corrective treatment for subluxation and all documentation required by Medicare was being maintained on file.
However, the documentation provided by the chiropractors for 94 services did not support the medical necessity of the services; 37 of these services had more than 90 days (approximately 3 months) between the date of initial treatment and the date of service, which may indicate that the services were maintenance therapy.
The Passage of Time Does Not Dictate the Need for Back Care
But, as mentioned above, CMS does not make any requirement that chiropractic treatment services with an AT designation have to occur within a 90-day window to be acceptable. And that is not a valid reason for rejecting a claim. The mere passage of time does not determine what is active treatment and what is maintenance treatment.
Is the Inspector General’s Report Anti-Chiropractic?
The tone of the Inspector General’s report seemed anti-chiropractic. Just from the language, it appears as if the Inspector General would be more comfortable if there were much less chiropractic treatment under Medicare policies.
Yet, the real scandal in back care, and pain care, in the United States is the continuing mistreatment and overtreatment of acute and chronic pain in primary care medical settings with opioids—which have led to almost 30,000 deaths per year in the United States.
One of the best ways to keep patients away from opioids in primary care settings is to route them to complementary and alternative care, including chiropractic. And multiple commentaries in medical journals have recommended expanding back care to include complementary and alternative care.
Some have recommended employing specially trained chiropractors and physical therapists as the main, front-line providers for low back pain. [See Donald Murphy’s two books on primary spine care providers}
So why is the Inspector General so hostile to chiropractic?
The same report by the Inspector General was discussed in an article at Medscape.com by Robert Lowes. That feature also included a section with 45 comments from MDs, DCs, and other healthcare providers.
“How are We to Care for Our Patients?”
A comment from a primary care MD—a general practitioner—stood out. “So we are no longer supposed to treat painful conditions such as headaches and back pain with opioids, and we are being encouraged to direct patients to the previously discouraged complementary modalities….which Medicare won’t pay for. Seems like Medicare needs to be brought up to date. And in the meantime, how are we to care for our patients?” asked Laura Shulman, MD.
Ironically, spinal manipulation has a better track record of safety and effectiveness than opioids in evidence-based guidelines on back pain. Yet, the Inspector General’s Office is on the warpath against chiropractic.
CMS Response: Where is the Medical Evidence to Support the Recommendations?
CMS did not seem impressed with this report—at least based on its letter in response. And CMS rejected one of the main recommendations (i.e. that CMS impose a limit on the number of chiropractic treatments it will underwrite).
The Inspector General recommended that CMS should “Determine whether should be a limit for the number of chiropractic services that Medicare will reimburse; if so, take appropriate action to put that limit into effect, and implement a system edit to disallow services in excess of that limit.”
CMS rejected this recommendation based on the existing scientific evidence. The following is an excerpt from the CMS letter in response to the Office of the Inspector General:
“CMS does not concur with the OIG recommendation. In order to implement this recommendation, CMS would need to develop a national coverage determination establishing a limit on the number of chiropractic services that are reasonable and necessary.
CMS is not aware of medical evidence that would support such a determination.”
Disclosures: None declared.
References:
- CMS Comments, in Office of the Inspector General Report, 2016;19–21; https://oig.hhs.gov/oas/reports/region9/91402033.pdf
- Davidson J, Medicare overpaid for most chiropractic services. Will patients have to repay?, Washington Post, October 26, 2016; www.washingtonpost . c o m / n e w s / p o w e r p o s t /wp/2016/10/26/medicare-overpaid-formost-chiropractic-services-willpatients-have-to-repay/.
- Donachie R, Medicare wasted $359 million on superfluous chiropractic treatments, Daily Caller, October 19, 2016; http://dailycaller.com/2016/10/19/ medicare-wasted-359-million-onsuperfluous-chiropractic-treatments/.
- Lowes R, Most Medicare claims from chiropractors improper, HHS says, Medscape, October 25, 2016; www.medscape.com/viewarticle/870910.
- Office of the Inspector General, Hundreds of millions in Medicare payments for chiropractic services did not comply with Medicare requirements, October, 2016; https://oig.hhs.gov/oas/reports/region9/91402033.pdf.
- Pianin E, Medicare Paid Chiropractors Bone-Chilling Millions for Bogus Billings, Fiscal Times, October 24, 2016;www.thefiscaltimes.com/2016/10/24/Medicare-Paid-Chiropractors-Bone-Chilling-Millions-Bogus-Billings.
- Shulman L, Comment Section, article by Lowes R, Most Medicare claims from Chiropractors improper, HHS says, Medscape, October 25, 2016; www. medscape.com/viewarticle/870910.
Post Script
Certainly it is powerful when the most astute editor in medical spine care comes to our defense as Mr. Mark Schoene did in this article. You may have noticed he wrote:
“Ironically, spinal manipulation has a better track record of safety and effectiveness than opioids in evidence-based guidelines on back pain. Yet, the Inspector General’s Office is on the warpath against chiropractic.”
Mr. Schoene did ask a good question that went unanswered: “So why is the Inspector General so hostile to chiropractic?”
That question is probably impossible to determine, but a good guess would be Daniel R. Levinson, Inspector General, like many attorneys, suffers from chirophobia after years of hearing medical propaganda, rubbing elbows with MDs (including HHS nominee Dr. Tom Price, orthopedist), and fake news about the supposed horrors of chiropractic care.
Considering the evidence supporting chiropractic care in this era of back pain, wouldn’t this be a good time to go on the offensive by publicly asking in the media, “Why is the Inspector General so hostile to chiropractic?”
We should embrace a debate with the IOG on this matter to clear the air.
Gone But Not Forgotten
Although the media’s focus is now on the allegedly fraud among chiropractors, the media seems to have a blind eye on the extensive fraud among MDs, surgeons, device manufacturers, hospitals and workers’ comp that constitute the bulk of medical fraud in this country.
As of March, 2015, Departments of Justice and Health and Human Services announce over $27.8 billion in returns from joint efforts to combat health care fraud.[2] Undoubtedly this sum in much higher now.
If the OIG and HHS want to stop medical fraud, it’s best to look at spine surgeons, which is not a new issue. According to “Medicare data cast spotlight on most prolific spinal surgeons,” experts have long been alarmed by the growth rate of spinal-fusion surgeries.
An analysis of new Medicare data by CBS News, “Tapping into controversial back surgeries,” shows a disproportionate number of the most risky and highest-paying procedures are being performed by a small group of high-volume spinal surgeons who perform the riskiest surgeries are also paid the most because they involve fusing more vertebrae together.
The analysis found that just 5% of all spinal surgeons performed 40% of Medicare surgical cases that fused four or more vertebrae. While the national average was 46 surgeries over the two year period, some did more than 460. While the average spine surgeon performed them on 7% of patients they saw, some did so on 35%.
There are many potential explanations as to why some surgeons recommend the highest-paying, yet riskiest surgeries far more often than do their peers, but the most obvious was noted in the CBS report that spinal-fusion surgery pays about five times more than less-risky alternatives, raising the belief doctors are letting financial considerations influence their recommendations.
From 2001 to 2010, an estimated 3.6 million spinal fusions were performed in the United States, with total charges of more than $287 billion. In patients covered by Medicare, the rate of complex spinal surgery has increased 15-fold since 2002,[3] making them more frequently performed than even hip replacements.
Medicare doesn’t have upfront approval for spinal fusions, but can recover money for surgery later deemed unnecessary. A report shows Medicare improperly spent $120 million on lumbar fusions in 2012.[4]
The main factors at play are the huge expenses. Hospitalization for spinal fusion surgeries alone accounts for over $40 billion annually,[5] which explains why administrators do not want chiropractors on staff—we would take too much money out of their pockets.
“But that’s just the hospital bill, without the surgeons’ or anesthesiologists’ fee, the MRI, the devices used in fusions (screws, cages), other operating room fees, and the postoperative rehab all add substantially to the final cost,” added renowned spine researcher, Rick Deyo, MD, MPH.[6]
Dr. Deyo suggested other possibilities for the rapid rise in fusion surgery:
- aggressive marketing of surgical implants like pedicle screws and cages;
- the rise in the number of paid consultants (“key opinion leaders”);
- alleged kickbacks from device manufacturers to surgeons;
- improvements in surgical and anesthesia techniques that might have expanded the pool of potential fusion surgery candidates, and
- a heavily entrenched, heavily promoted treatment enterprise not willing to give up this lucrative market share.[7]
MAC to the Rescue
Another point omitted by Mr. Schoene was the fact some Medicare Accounting Contractors (MAC) have now scrutinized unnecessary medical spine care, specifically spine fusions, that are not following the guideline to use conservative care first.
These tighter indications for spinal fusion and a challenging reimbursement market led to predictions that in the United States’ share of the spinal fusion market will shrink by 8% from 71 percent in 2013 to 63 percent in 2020.[8]
I wrote about this in my article, “Climbing the Ladder of Opportunity”:
Part One was published in Dynamic Chiropractic on March 6, 2014. Part Two was published on April 1, 2014 (no kidding!).
The following is an excerpt from my article:
Apparently the hospitals’ “open-door” policy for any surgeon to do any surgery on anyone for any reason is coming to an end. Perhaps of most significance to chiropractors is the requirement that patients scheduled for elective spinal fusion procedures must have well-documented attempts at various forms of conservative care beforehand, just as the Agency for Health Care Policy & Research (AHCPR) guideline #14 on acute low back pain in adults recommended twenty years ago.[7]
According to the LCD from First Coast Service Options, Inc., “Coverage Indications Limitations and/or Medical Necessity” states:
“Low back pain is a common disorder affecting 80% of people at some point in their lives. Causes stem from a wide variety of conditions, although in some cases no specific etiology is identified. Age-related intervertebral disc degeneration, typically resulting in degeneration of the discs themselves, facet joint arthrosis, and segmental instability are causative factors. Initial management can include rest, exercise program, avoidance of activities that aggravate pain, application of heat/cold modalities, pharmacotherapy, local injections, lumbar bracing, chiropractic manipulation, and physical therapy. When conservative therapy (non-surgical medical management) is unsuccessful after at least 3 to 12 months, depending on the diagnosis, lumbar spinal fusion may be considered for certain conditions.”
According to Mr. Schuck, when any MAC performs a Spinal Fusion-Medical Necessity and Coding Analysis, they expect documentation in the patients’ medical charts to reflect the appropriate diagnosis and include the following:
- Pre-procedure radiological findings or mention of the radiology report result in the medical record
- Failed conservative measures/treatment prior to surgery
- Documentation of duration of pain and/or impairment of function
- Physical exam documenting the functional pathology
- Documentation of instability if applicable
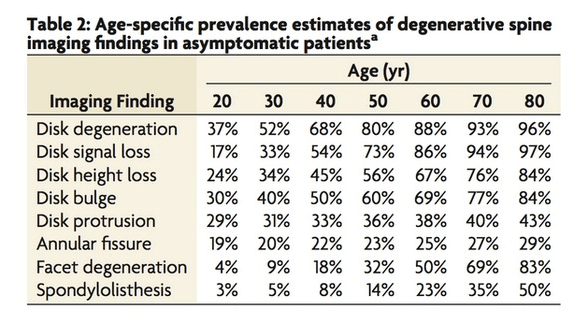
Finally, CMS and some private payors, such as the North Carolina BC/BS,[8] now basically realize that “bad discs” are “red herrings,” adroitly described by Donald Murphy, DC,[9] because the evidence does not support a purely pathoanatomical model for spine-related disorders because they also appear in pain-free people.[10]
[Let me add a chart from the Mayo Clinic that also found “bad discs” in pain-free people, yet these uninformed patients will still fall prey to unethical surgeons who convince them the “bad discs” automatically calls for fusion.]
The Ax Man Cometh
This decision is a huge step up our ladder of opportunity when payors are denying payment for inefficient medical spine care based upon evidence-based reasons that will certainly reduce the tsunami of unnecessary spine surgeries.
This past October, 2013, an update from Palmetto Government Benefits Administrators (GBA), another regional MAC, revealed the results of their pre-payment service review of “Medicare-severity” diagnosis related groups (MS-DRG).
Palmetto’s findings for MS-DRG 460 (spine fusions) in North Carolina, Virginia, and West Virginia exposed high error rates regarding lack of medical necessity documentation, no doubt causing a panic among spine surgeons and hospitals when this Palmetto MAC refused to pay them.
According to data published on the Palmetto GBA website, a pre-payment review of 251 claims in North Carolina, Virginia, and West Virginia led to 168 claims either completely or partially denied. The total reviewed was $6,356,890 and $4,141,771 was denied, resulting in a charge denial rate of 65%.[11]
Imagine the shock wave when payment for 65% of fusions were denied! Finally, there appears to be some sanity in the medical spine industry, at least by some payors at CMS.
According to Barry Zeman, former hospital CEO and consultant for Specialty Healthcare Advisers, “Today, with greater pre-payment review authority being given to MACs, it’s creating a whole new ball game. Under a pre-payment review, MACs have greater authority to examine the medical necessity documentation prior to making payment…With ICD-10, the days of performing cases with less than adequate documentation are gone forever.”[12]
Too High a Price
So, can we chiropractors hope this trend to evidence-based conservative care continues in Medicare or can we expect Dr. Tom Price to ignore the data and give the green flag to his spine colleagues?
Considering orthopedic surgeons donate $928k to Dr. Tom Price over 12-year period and specialists have donated at least $3.1 million over the past 13 years to Dr. Price’s political committees, I think the answer is obvious.
The price of pain also extends to our legislators. NM Hadler, MD, in his book, “Stabbed in the Back”, wrote, “The pen may be mightier than the sword, but it is not mightier than the dollar,”[9] and the AMA and Big Pharma has plenty of dollars to wield its sword on Capitol Hill.
As we know in Washington, D.C., money equates to power.[10]
Little do people know the medical-industrial complex spends four times as much on lobbying as the No. 2 Beltway spender, the much-feared military-industrial complex, which explains one reason why Harper’s Magazine once called the AMA as “the most terrifying trade association on earth.”[11]
According to OpenSecrets.org, the annual lobbying on health legislative issues in 2015 was $381,223,403 ($712,567 per congressman) of which Big Pharma alone spent $178,863,490 ($334,324 per congressman).[12] The total spent in 2015 was down from $556,002,269 ($1,039,256 per congressman) at the height of the Obamacare debate.
The total contributions by health professionals to federal candidates and parties amounted to $70,377,772 ($131,547 per congressman) for the election cycle ending in 2014. The AMA alone contributed $19,650,000 in 2014 ($36,728 per congressman).
In comparison, all chiropractic contributions amounted to a paltry $527,832 ($986 per congressman).
There is simply too much money for Congress to criticize either Big Pharma or the medical dealers who pad their pockets.
Unless there is a moral epiphany among Trump’s administration, we should expect the worse of times rather than the best of times in our future.
[1] http://www.thefiscaltimes.com/2016/06/23/Doctors-and-Nurses-Charged-Massive-900-Million-Medicare-Fraud
[2] https://www.hhs.gov/about/news/2015/03/19/departments-of-justice-and-health-and-human-services-announce-over-27-point-8-billion-in-returns-from-joint-efforts-to-combat-health-care-fraud.html
[3] https://www.spineuniverse.com/professional/news/medicare-payments-spine-surgery-vary-across-nation
[4] http://www.beckersspine.com/spine/item/21289-cigna-reports-15-of-spinal-fusion-customers-undergo-2nd-surgery-5-key-points.html
[5] HCUPnet. Agency for Healthcare Research and Quality. Available at: http://hcupnet.ahrq.gov/HCUPnet.jsp . Accessed October 30, 2014.
[6] Private communication with JC Smith, 3/19/2015.
[7] Spinal Fusion for DDD a Growth Industry for Two Decades—Despite an Uncertain Evidence Base, BackLetter: April 2015 – Volume 30 – Issue 4 – p 39–41
[8] http://www.beckersspine.com/spine/item/21248-u-s-spinal-fusion-market-share-to-drop-8-by-2020-china-to-grow-5
[9] Hadler, NM, Stabbed in the Back; confronting back pain in an overtreated society, University of North Carolina Press, 2009, pp. 88
[10] Steven Brill, What I Learned From My $190,000 Surgery, TIME, Jan. 8, 2015
[11] M Mayer, ibid. p. 76.