Chiropractors Have Your Back
By
JCS
Americans love any story about the underdog, especially when it raises your social consciousness as we’ve seen recently with the hit movie/book, The Help, which will forever change the way anyone views the harsh reality of the Jim Crow South before the Civil Rights movement took hold.
Certainly, the media has hastened the social changes we now see. The recent 63rd Primetime Emmy Awards also brought to the forefront the issue of social tolerance about homosexuality when the Modern Family won five awards. As well, the military’s “don’t ask, don’t tell” rule since the Clinton administration has been replaced with a policy designed to be blind to sexual orientation.
Despite the growing acceptance of diversity in all facets of American life, there remains one area that has not been discussed nor have we seen much progress—discrimination in American healthcare and, specifically, the role of chiropractors.
Once libeled as quackery by the AMA, which eventually found itself at the wrong end of a subsequent antitrust case for defaming and boycotting chiropractors in public hospitals, the chiropractic profession has had a difficult time shaking this imagery. No movie or television program, nor cable news programs have championed the prejudice faced by chiropractors over the last century.
This is not to say chiropractors have not made huge strides since the early 20th century when over 12,000 chiropractors were arrested for supposedly practicing medicine without a license. Despite the strides chiropractors have made, the lack of sympathetic media programs have failed to enlighten the public about the discrimination they faced. In fact, it can be argued that the medical profession’s total control of cable news has perpetuated the absence of awareness of the plight of chiropractic.
In fact, the accusation of medical quackery was a bogus charge from the start since chiropractors never practiced with drugs or surgery, but they did practice a manipulative art stemming from antiquity dating back 3,000 years to the great Egyptian physician, Imhotep. Similar practitioners in medieval Europe were coined as bonesetters in 1510, which eventually spread to North America. These bonesetters usually belonged to the peasantry, and the art was passed on in the same families from parent to child for many generations.[1]
The art of spinal manipulation, the mainstay of chiropractic care, is certainly not a new healing treatment. Nearly every civilization from Asia to Europe to indigenous native societies in the West[2], such as the Mayan civilization in Guatemala to Montana’s Crow Indian healers, have had “bone-setters” who popped, pulled, tramped, twisted, or “racked” (as DD Palmer, the founder of chiropractic, described the “knack” of adjusting) the spine as well as other joints to relieve pain, impairment, and disability.
The history of spinal biomechanics has its origins in antiquity. Egyptian documents written in the seventeenth century B.C. describe the difference between cervical sprain, fracture, and fracture-dislocation. In ancient Greece, Hippocrates provided recorded more evidence in his book, On Joints, written in the fifth century BC. This described the practice of spinal manipulation by physical means such as traction or local pressure to correct spinal deformities. [3]
During the Renaissance, Leonardo da Vinci (1452-1519) accurately described the anatomy of the spine and was perhaps the first to investigate spinal stability. The first comprehensive treatise on biomechanics, De Motu Animalium, was published in 1680 by Giovanni Borelli, who is often called the “Father of Spinal Biomechanics.”[4]
A rare book by George Matthews Bennett, The Art of the Bone-Setter (London: Thos. Murby & Co., 1884), gives an excellent history of bonesetters in England, Wales, and Scotland. One of the earliest English books on bonesetting was The Compleat Bonesetter by Friar Thomas Moulton (London: Thos. Rooks, 1665, pp. 20-21). Throughout Europe, the men and women who practiced bonesetting learned from others and honed their skills through practical experience. The skill was an art taught via hands-on training. [5]
Bone-setter Richard Hutton gained notoriety in London in the 1800s when he relieved the long-standing suffering of the Honorable Spencer Ponsonby, a son of an Earl and a prominent cricket player of tdhe time. It is rumored that even Queen Victoria, who suffered with migraines, was treated by a spinal manipulator. [6] Queen Victoria was also treated for rheumatic pains with Swedish massage and was so delighted with her results that the Royal Crown rewarded the practitioners with a school called the Swedish Institute which opened in London in 1838.[7] History makes clear that hands-on therapies have been used throughout recorded history to provide relief for people suffering with pain, discomfort, and health problems.
The Sweets of South County, Rhode Island, were among the original bonesetters in colonial America. [8] Of Welsh extraction the Sweets were an old Rhode Island family whose progenitor, John Sweet, came to the state from Salem, Massachusetts in 1637. The father usually selected one or two of his sons and instructed them in bonesetting. The Sweets did not deem this a magical thing, but more of an inherited knowledge acquired from their elders.
Dr. Benoni Sweet, born in 1663 and died in 1751 at the age of 90, was also known as “Captain Sweet” as he was called by his neighbors since in his early days he had been an officer in the British Army where “his skill in bonesetting was of high repute in Rhode Island and in Eastern Connecticut,” as reported in the New York Times on April 4, 1874 in an article “Distinguished Bone-Setters.”
During the Revolutionary War, his son, Dr. Job Sweet, born in 1724 and died in 1840 at the age of 80, was sent to Newport to set the bones of French officers, an operation their own doctors would not attempt. After the war, Colonel Aaron Burr, later Vice-President of the United States, sent for him to help his daughter, Theodosia, who had a dislocated hipbone.
Other than lay people who practiced bone-setting, the first academic investigation of this art of spinal manipulation began in 1874with Andrew Taylor Still, MD, when he developed the principles of osteopathy. In 1894 he secured the charter of the “American School of Osteopathy” in Kirksville, Missouri. Dr. Still He believed that diseases caused by mechanical interference with nerve and blood supply were curable by manipulation of “deranged, displaced bones, nerves, muscles—removing all obstructions—thereby setting the machinery of life moving.”[9]
Simultaneously in Davenport, Iowa, Daniel David (“DD”) Palmer began his health care practice as a magnetic healer in 1886 when he was 41 years old. Apparently DD Palmer had visited Dr. Still at his home, suggesting to some that Palmer had duplicated Still’s methods of manipulation.[10] Palmer would later write that his chiropractic techniques were totally different and that chiropractic had a different science and philosophy than osteopathy. The fundamental belief that structure affected function would remain similar for decades until osteopathy was absorbed by medicine. Palmer did claim to be the first to use the levers of the vertebrae to make specific “adjustments” to the spine rather than crude, regional “manipulations” as osteopaths of his time were doing. This difference in treatment, along with a different neurogenic explanation of health and disease causation, would become a legal turning point in the persecution of chiropractors.
The recorded origin of chiropractic began in 1895 when DD Palmer is credited to have reinvented the art of spinal manipulation or spinal “adjustment,” as he preferred. He would later admit that “The Chiropractic method was developed by me, not discovered.”[11]
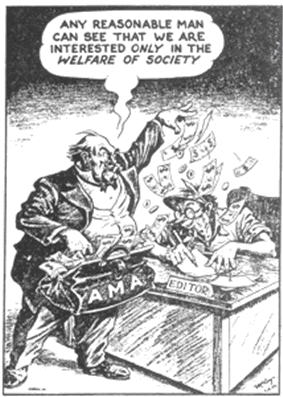
The medical attack on chiropractors was simply a ruse to create a medical monopoly. The medical tyranny essentially began in 1910 after the Flexner Report[12] resulted in the closing of many medical, homeopathic, and osteopathic schools. The Flexner Report used the nonprofit, federally subsidized university hospital setting as the new teaching facility of the medical profession, with Johns Hopkins as the model school, eventually gaining control of federal healthcare research and student aid.[13] This was the insidious second step by the AMA to become an invisible branch of government with the Flexner Report in one hand and the purse strings for healthcare in the other hand.
Two years later the fledging medical monarchy went on the offensive through the establishment of its Propaganda Department that was specifically dedicated to attacking any and all unconventional medical treatments and anyone (including MDs) who practiced them, namely the chiropractors, naturopaths, homeopaths, and original osteopaths.
Medical sociologist Paul Starr wrote in his Pulitzer Prize-winning book, The Social Transformation of American Medicine,[14] that as a result of the Flexner Report, the AMA presumed to have cultural authority to invoke its force upon both the medical profession and competing health professions like homeopathy, osteopathy, and chiropractic.
The AMA Council became a national accrediting agency for medical schools, as an increasing number of states adopted its judgments of unacceptable institutions…Even though no legislative body ever set up…the AMA Council on Medical Education, their decisions came to have the force of law.[15] (emphasis added)
Today the chiropractic profession is the third-largest physician-level health profession in the world, only behind MDs and dentists, but its image still suffers from the illegal defamation campaign by the AMA. Even celebrated national columnist Ann Landers was on the payroll of the AMA to slander chiropractors, a fact revealed in an antitrust lawsuit filed by five chiropractors in 1976 in federal court in Chicago (Wilk et al. v. AMA et al.).
Despite this landmark legal victory, even the judge spoke of the damage to the reputation of chiropractors:
The activities of the AMA undoubtedly have injured the reputation of chiropractors generally…In my judgment, this injury continues to the present time and likely continues to adversely affect the plaintiffs. The AMA has never made any attempt to publicly repair the damage the boycott did to chiropractors’ reputations.[16]
The medical witch hunt against all competitors, especially chiropractors, has left an indelible stain on mindset of many people, but this stain has never been removed despite the court victory and recent research, most notably, the USPHS’s Agency on Health Care Policy & Research (AHCPR) in 1994 listing spinal manipulation as a preferred treatment for acute low back pain.
Indeed, a 1984 public survey in Oklahoma sought public opinion of chiropractors: “to many respondents, chiropractors are seen as being fine for many people in the community, but,” one respondent said, “I wouldn’t want my daughter to marry one.”[17]
This bias makes one wonder the source of this prejudice. Although racism and sexism have diffuse origins in history, the medical persecution of chiropractic can be traced back to one man, Morris Fishbein, MD, who was the voice and the face of the AMA as its executive director from 1924 to 1949. For a quarter of a century, this one man was dubbed the Medical Mussolini by his own contemporaries for his tyrannical leadership that led a campaign to eliminate any and all competition.
Fishbein’s goal was clearly stated in his 1925 book: “Scientific medicine absorbs from them that which is good, if there is any good, and then they die.” [18] And many did die or were arrested—the first victims were the homeopaths and naturopaths, then the original osteopaths and chiropractors were attacked, barely surviving although scathed.
According to historian Russell W. Gibbons, chiropractors felt the brunt as one of the first grass roots movements in America:
…like abolitionists, chiropractors were systematically persecuted and driven from town to town. Like the feminists and suffragettes, chiropractors were made objects of ridicule. And like the civil rights workers of more recent times, chiropractors were intimidated and subverted by agents and provocateurs. In the finest tradition of reform movements, they were imprisoned for their beliefs. [19]
Later the AMA turned its guns against dentists, optometrists, and, most recently, nurse-practitioners. Without question, the AMA has fought to maintain its iron-fisted control of the American healthcare delivery system. Diversity and inclusion has never been a trademark of the AMA.
Since every war needs to be funded, so too did the medical war against chiropractors. When Fishbein took control, like all other trade associations, the AMA was poorly funded by only dues and journal subscriptions for revenue, and needed outside sources of income to bolster its war coffer. To accomplish his goal, Fishbein was up to his neck in spurious moneymaking efforts, most notably, accepting tobacco ads in his journals to fuel his warfare.
Tobacco became the cash cow for the medical association, and it ultimately revealed Fishbein’s true intention—to make money by exploiting the image of the medical profession as “guardians of health” at the expense of patients’ health by withholding the truth about the damage from tobacco.
These lucrative ads made the Journal of the American Medical Association the most profitable magazine in the world and the AMA the most powerful trade association. This profit fueled the increasing political power of the AMA to thwart opposition and to influence the media and politicians.
Fishbein commented on this easy money, and suggested it was only a fraction of what he could earn:
The JAMA netted a non-taxable $1,400,000 in 1948…the 1948 accounting showed revenue of $4,858,000 from “periodical subscriptions and advertising” out of $5,166,000 from all sources. “I turn down as much advertising as I accept—over a million a year,” the editor [Fishbein] said. [20]
Apparently the ploy of “public safety” used by the AMA to condemn chiropractors was only a smokescreen since the AMA obviously had no real concern for public safety by endorsing the use of tobacco. Indeed, as Harper’s Magazine described in 1949, it was tobacco money that initially transformed the AMA from a “panty waist organization into the most terrifying trade association on earth.”[21]
Under Fishbein’s reign, the tobacco companies became the largest advertiser in JAMA and in various local medical society publications. The AMA allowed the image of physicians in these ads despite the fact that by the 1930s medical journals were already publishing studies associating smoking with lung cancer.[22]
Fishbein was instrumental in helping tobacco companies conduct supposedly “scientific” testing to substantiate their claims. Some of the ad claims that Fishbein approved for inclusion in JAMA were:
- “Not a cough in a carload” (Old Gold cigarettes).
- “Not one single case of throat irritation due to smoking Camels”.
- “More doctors smoke Camels than any other cigarette.”
- “Just what the doctor ordered” (L&M cigarettes).
- “For digestion’s sake, smoke Camels” (Allegedly the magical Camel cigarettes would “stimulate the flow of digestive fluids”).

The JAMA published its first cigarette advertisement in 1933, stating that it had done so only “after careful consideration of the extent to which cigarettes were used by physicians in practice.”[23] The same year, Chesterfield began running ads in the New York State Journal of Medicine, with the claim that its cigarettes were “Just as pure as the water you drink… and practically untouched by human hands.”[24]
This ruse exemplifies the deceitfulness of the AMA to do whatever it could to make money to fuel its political war chest. For the AMA to lie to the public about the safety of cigarettes and actually suggest tobacco was healthy while at the same time defame chiropractic as dangerous seriously questioned the integrity of Fishbein and the AMA executives.
In the 1950s when overwhelming evidence of the causation of lung cancer by smoking reached the public did the Journal stop accepting tobacco ads, though Fishbein was by then serving as a highly paid consultant to the Lorillard tobacco company after his ouster from the AMA.[25]
Yet few in the media questioned this obvious skewed behavior, illustrating the ability of the AMA to defame its opponents and get away with it as the so-called guardians of Americans’ health. Indeed, no one dare question the powerful AMA on any health matter as long as the war coffers afforded medical persuasion, not unlike today with AMA Political Action Committee, whose website states as of August 31, 2011 available funds of $1,950,819.62.[26]
In his book, Free to Choose, economist Milton Friedman said “the AMA has engaged in extensive litigation charging chiropractors and osteopathic physicians with the unlicensed practice of medicine, in an attempt to restrict them to as narrow an area as possible.”[27]
The AMA remains the dominant power in healthcare today with its political action war chest to suppress all competitors. Without question, the AMA has been the proverbial wolf in sheep’s clothing masquerading as the guardian of health when, in reality, it has been the guardian of its own wealth. It is time for the public to see the AMA for what it really is: “the most terrifying [and wealthiest] trade association on earth.”[28]
Finally in 1976, the wolf’s clothing would be stripped away when a few courageous chiropractors took the AMA to task in a federal antitrust trial in Chicago. After decades of warfare tormenting the chiropractic profession and its patients, it was time to hold the AMA’s feet to the fire in courtroom cross-examination. This trial, Wilk et al. v. AMA et al., would blow the AMA’s cover and disprove their allegations against chiropractic, making for one of the most interesting trials in medical history, and a trial the AMA would prefer remain untold.
New Spine Care Paradigm
Not only was the AMA proven guilty in its campaign to “contain and eliminate”[29] the chiropractic profession, the scientific community today has rebuked the epidemic of spine surgeries.
Ironically, after decades of proclaiming chiropractic to be “unscientific,” new facts are emerging in international guidelines that non-surgical methods, principally chiropractic, massage therapy, active rehab, and acupuncture are the preferred initial methods of treatment and the medical methods—drugs, epidural shots, and spine fusions—are consider the last resorts.
The recommendation for spinal manipulative therapy before surgery is not new. Beginning with the US Public Health Service’s AHCPR guideline on acute low back pain in 1994[30], more recent guidelines including the North American Spine Society[31], the American Pain Society[32], and the Milliman Care Guidelines®[33] recommend spinal manipulation therapy as a first avenue for treatment and spine surgery as the last option, a point lost to most MDs.
The North American Spine Society (NASS) has now published online a Public Education Series that includes “Spinal Fusion.” Remarkably, this explanation proved to be very accurate, including the opinion that “Fusion under these conditions is usually viewed as a last resort and should be considered only after other conservative (non-surgical) measures have failed.”
The admission by NASS that fusion should be a last resort is a huge warning that has been unheard by the public since most surgeons refuse to tell them. The NASS again admitted that spinal manipulation should be considered before surgery in the October, 2010, edition of The Spine Journal:
Several RCTs (random controlled trials) have been conducted to assess the efficacy of SMT (spinal manipulative therapy) for acute LBP (low back pain) using various methods. Results from most studies suggest that 5 to 10 sessions of SMT administered over 2 to 4 weeks achieve equivalent or superior improvement in pain and function when compared with other commonly used interventions, such as physical modalities, medication, education, or exercise, for short, intermediate, and long-term follow-up. Spine care clinicians should discuss the role of SMT as a treatment option for patients with acute LBP who do not find adequate symptomatic relief with self-care and education alone.[34]
Similar studies in the U.S.[35], U.K.[36], Canada[37], and Denmark[38] all concluded that back surgeries were excessive, and conservative care such as spinal manipulative therapy and active rehab were the best initial approaches to the vast majority of low back pain problems, including those with radiculopathy.
Recently a study by McMorland et al. showed that spinal manipulation was just as effective as microdiskectomy for patients with sciatica secondary to lumbar disc herniation. The authors found sixty percent of patients with sciatica benefited from spinal manipulation. [39]
Richard Deyo, MD, MPH, mentioned chiropractic as a solution: “Chiropractic is the most common choice, and evidence accumulates that spinal manipulation may indeed be an effective short-term pain remedy for patients with recent back problems.”[40]
Gordon Waddell, DSc, MD, FRCS, author, and director of an orthopedic surgical clinic for over 20 years in Glasgow, Scotland, also suggested: “There is now considerable evidence that manipulation can be an effective method of providing symptomatic relief for some patients with acute low back pain.”[41]
Disc Theory is Dead
Although most MDs and many in the public remain convinced that a disc problem requires surgery, new research refutes this old premise. Just as the public was badly misled by the AMA in regards to chiropractic care, medical spine care has also now been shown to be misleading in its diagnosis and treatment.
Research now casts a shadow over the medical belief that back pain is due primarily to disc problems. After decades relying on the abnormal disc as the cause of back pain and the justification for spine surgery, MRI research has now disproved this notion to the dismay of spine surgeons although a cover-up currently prevails to squash this notion.
The fundamental flaw of medical spine diagnosis rests with the emphasis on MRIs to detect pathoanatomical disorders (disc abnormalities, arthritis, bone spurs) rather than the emphasis on pathophysiologic disorders (malfunctioning of the spine as a weight-bearing unit due to a combination of joint dysfunction, vertebral misalignment, loss of flexibility, muscle weakness, and axial compression). What matters most, as studies now confirm, is how the spine functions, not just the amount of anatomical degeneration or disc abnormalities.
The first study on the disassociation between disc abnormalities and back pain was done by Emory researcher, Scott Boden, MD. This renaissance in spine diagnosis began in 1990 when research by Boden et al.[42] followed in 1994 by a supportive study by Maureen Jensen et al.[43] found no clear correlation between disc abnormalities and back pain.
With that in mind, research shows the abundance of MRI scans leads to excessive back surgeries. According to Stanford University Medical Center, patients who live in areas with more MRI scanners are more likely to undergo spine surgery. [44] “The worry is that many people will not benefit from the surgery, so heading in this direction is concerning,” said senior author Laurence Baker, PhD.[45]
Yet this dubious theory remains very much alive today via the “herniated/degenerative/slipped/abnormal disc” diagnosis used by spine surgeons despite the fact that there are many people with pain who have perfectly healthy discs, and vice versa, many asymptomatic people have severe pathoanatomical issues. Indeed, Richard Deyo, MD, MPH, has dubbed abnormal discs as “incidentalomas” since pain-free people have them and they are incidental to the underlying problem.[46]
The revelation about unnecessary fusions continues to appear in the mainstream media including a recent cover story in Newsweek magazine, “No! The One Word that Can Save Your Life” by Sharon Begley (August 22, 2011). The article spoke about many unnecessary surgeries, including spine surgery based on the abnormal disc theory:
“That’s because the ‘abnormalities’ seen in an MRI often have nothing to do with the back pain (people without pain have them too), but seeing something on a scan makes a physician feel compelled to get rid of it. “There is a long-standing fallacy among physicians that if you find something different from what you perceive to be ‘normal,’ then it must be the cause of the patient’s problem,” says UNC’s Nortin M. Hadler, MD.”
“In fact,” according to Richard Deyo, “back surgery rates are highest where MRIs are the highest. In a randomized trial, we found that doing an MRI instead of a plain x-ray led to more back surgery, but didn’t improve the overall results of treatment.”[47] Indisputably, MRI scans are often used as effective selling points that have greatly increased the number of unnecessary surgery.
In my clinic I often hear patients with failed back surgery tell me, “But the doctor showed me the herniated/degenerated disc on the MRI” to warrant fusion. After fusion surgery with metal hardware implanted in their spines, they wonder why they are still in pain, if not more pain than before. I simply suggest to them that the source of their pain may not be slipped discs as much as slipped spinal joints.
I might add there are some unscrupulous spine surgeons who actually lie to patients. “If you don’t have my fusion, you may be paralyzed, and if you go to a chiropractor, he will paralyze you.” If I had a nickel for every time I’ve heard this lie, I would be rich. In fact, I know of no one who is paralyzed from a disc herniation and chiropractors have the lowest malpractice rates of all spine doctors. Yet these medical lies frighten many people into unnecessary spine fusions.
New research now questions the long-term benefits of spinal fusions and diskectomies. An extensive 2006 study, “The Spine Patient Outcomes Research Trial (SPORT),” led by James N. Weinstein, Director of the Dartmouth Institute for Health Policy and Clinical Practice, shows that patients with low back and leg pain who underwent spinal discectomy surgery fared no better two years later than those who used non-invasive therapies.[48]
The SPORT study is the latest to suggest that American medicine is losing its battle against back pain and that many medical treatments may be ineffective or overused. Dr. Weinstein said the rapid growth in surgical procedures, coupled with the lack of hard evidence, points to the need to spell out all the risks and benefits for patients and let them choose.
“As in most of medicine, there isn’t as much evidence as we would like,” said Dr. Weinstein. “We need to be clear that there is a choice of treatments,” he said, and “that one isn’t necessarily better than the other.”[49]
In an interview in The New York Times, Eugene Carragee, professor of orthopedic surgery at Stanford and an investigator in the SPORT study, admitted the “proliferation of risky and expensive practice beyond reasonable supporting evidence is commonly mentioned as a fundamental failing of medical practice in the United States.”[50] He also noted “there is good evidence that simpler methods are highly effective.”[51]
Indeed, there are “simpler methods” that are highly effective for back pain, namely chiropractic care as many studies have indicated. Not only are simpler methods preferable in most cases, a 2005 study from Switzerland suggests that a surgeon’s optimistic attitude may be unrealistic compared to actual patient outcomes.[52]
According to a University of Lausanne study done of 197 patients who had surgery for low back pain or sciatica, surgeons forecasted “excellent or at least moderate improvement” for nearly all (99 percent) of patients. Rather than the optimistic 99 percent prediction by surgeons, in fact, the majority (56 percent) of the patients showed no significant improvements in their general health a year after their back surgery.
The Swiss team concluded that “surgeons tended to give overly optimistic predictions that were not correlated with patient outcome.” The researchers believed the “more optimistic physician expectation was associated with better improvement of psychological dimensions,” what they referred to as the “curabo effect.” The power of the surgeon’s suggestion, not unlike the “placebo effect,” makes patients think they improved without any real corrective intervention.
The call for restraint in spine surgery has grown louder since spine fusion is now considered by many medical researchers among the most questionable as well as among the most expensive surgery in America. This is the professional opinion of many orthopedists, not only mine.
Gordon Waddell admits that back surgery is mostly ineffective and disabling:
“Low back pain has been a 20th century health care disaster. Medical care certainly has not solved the everyday symptom of low back pain and even may be reinforcing and exacerbating the problem…It [back surgery] has been accused of leaving more tragic human wreckage in its wake than any other operation in history.”[53]
The editors of The BACKLETTER®, a newsletter from the Department of Orthopedic Surgery at Georgetown Medical Center in Washington, DC, agree with his frustration with the medical approach:
The world of spinal medicine, unfortunately, is producing patients with failed back surgery syndrome at an alarming rate…There is growing frustration over the lack of progress in the surgical treatment of degenerative disc disease. Despite a steady stream of technological innovations over the past 15 years—from pedical screws to fusion cages to artificial discs—there is little evidence that patient outcomes have improved…Many would like to see an entirely new research effort in this area, to see whether degenerative disc disease and/or discogenic pain are actually diagnosable and treatable conditions.[54],[55]
Dr. Deyo commented in an article in the New York Times when he mentioned the failings of the medical model for back pain:
I think the truth is we have perhaps oversold what we have to offer. All the imaging we do, all the drug treatments, all the injections, all the operations have benefit for some patients. But in each of these situations, we’ve begun using those tests and treatments more widely than science would really support. [56]
Another turning point occurred when Blue Cross Blue Shield of North Carolina announced in January, 2011, that it would no longer pay for spinal fusion for back pain in the presence of only disc degeneration or disc herniation. This is a huge policy change that will hopefully have a ripple effect among all state BC/BS and other insurance companies to curtail payment for this epidemic of ineffective disc fusion surgery. [57]
Unquestionably, the need for a paradigm shift in spine care is gaining public attention. The Wall Street Journal, New York Times, NPR, MSNBC, and the Bloomberg News have exposed the ineffectiveness of spine surgery, the greed of many surgeons, the financial influence by Medtronic, and questionable disc theory behind spinal surgery as well as wasted revenues of these unnecessary surgeries.
For example, here are a few recent media exposés on spine surgery:
- “Surgery May Not Be the Answer to an Aching Back,” by Joanne Silberner, NPR, April 6, 2010.
- “Back Surgery May Backfire on Patients in Pain,” by Linda Carroll, MSNBC, Nov. 14, 2010
- “Top Spine Surgeons Reap Royalties, Medicare Bounty,” by John Carreyrou and Tom McGinty, Wall St. Journal, Dec. 20, 2010
- “Highest-Paid U.S. Doctors Get Rich with Fusion Surgery Debunked by Studies” by Peter Waldman and David Armstrong, Bloomberg News, Dec. 30, 2010.
- “Spinal Fusions May Cause More Harm Than Good,” by Terrance Pagel, Daily Health Report, Jan. 20, 2011
- “Medicare Records Reveal Trail of Troubling Surgeries” by John Carreyrou and Tom McGinty, Wall St. Journal, March 29, 2011
- “Spine Experts Repudiate Medtronic Studies” by Barry Meier and Duff Wilson, June 28, 2011, New York Times
Obviously the spine surgery business is now a huge public scandal. Moreover, this has led to thousands of unnecessary spine surgeries performed each year costing millions in lost work days/disability, billions of dollars in medical expense, as well as the incalculable human toll in suffering and depression by patients who never needed a spinal fusion and now must live with interminable pain. This also contributes to the drug addiction problem we now face in the so-called “hillbilly heroin” epidemic of patients addicted to opiates often due to failed back surgeries.
After nearly 100 years of warfare by the medical profession against chiropractors, the table as turned with the medical men in a very precarious situation—its defamation of chiropractors was shown to be bogus, its own disc theory disproved, and spine surgeries to be excessive and ineffective.
While it may take time for many Americans to adjust their social attitudes, just as many Southerners have done in regards to racism, the change toward chiropractic care in the very conservative medical world is increasing as more than 20 million Americans today enjoy this natural method to better health.
As the premier non-drug, non-surgical primary spine practitioners, chiropractors have your back, just as they have for over 100 years. After a century of war with the medical profession, research and guidelines now support chiropractic care as the first avenue of treatment in spine care.
[1] Scott Haldeman, Principles and Practice of Chiropractic, Appleton & Lange, (1992): 4.
[2] WH Dorn, “Indian Lore: Crude Us Of Chiropractic Fundamentals Centuries Ago,” Journal of Chiropractic. (NCA) 4/3 (1935): 17-8.
[3] Haldeman, Ibid. p. 7.
[4] Sanan Abhay, M.D., S. Setti Rengachary, M.D., “The History of Spinal Biomechanics,” Neurosurgery 39 (1996):657-69.
[5] Abhay Sanan, ibid. p. 657.
[7] MP Cassar, “Massage Made Easy: 100 Great Ways To Beat Stress, Relieve Aches And Pains And Tone Key Areas Of Your Body,” Allentown: People’s Medical Society. (1994).
[8] Martha R. McPartland, “The Bonesetter Sweets of South County, Rhode Island,” YANKEE, January 1968.
[9]Andrew Taylor Still, Autobiography —With a History of the Discovery and Development of the Science of Osteopathy. (New York: Arno Press, 1972; New York Times).
[10] Louis S. Reed, The Healing Cults: A Study of Sectarian Medical Practice; Its Extent, Causes, And Control, University of Chicago Press, 1932, p. 38.
[11] DD Palmer, The Chiropractor’s Adjuster: The Text-Book of the Science, Art and Philosophy of Chiropractic (Portland, Oregon: Portland Printing House) (1910): p. 581.
[12] The Flexner Report was published in 1910 under the aegis of the Carnegie Foundation and called on American medical schools to enact higher admission and graduation standards, and to adhere strictly to the protocols of mainstream medical science in their teaching and research.
[13] C Lerner, ‘Report on the history of chiropractic’ L.E. Lee papers, Palmer College Library Archives
[14] P Starr, The Social Transformation of American Medicine, New York: Basic Books, (1982).
[15] Ibid.
[16] Opinion p. 10
[17] “Attitudes Toward Chiropractic Health Care in Oklahoma,” Welling & Company and Oklahoma Chiropractic Research Foundation in cooperation with the Chiropractic Association of Oklahoma (1984)
[18] M Fishbein, Medical Follies, New York, Boni & Liveright (1925):43.
[19] R Gibbons, ibid. p. 67.
[20] MS Mayer, “The Rise and Fall of Dr. Fishbein,” Harper’s Magazine, (Nov. 1949): 76-85.
[21] Mayer, ibid. p. 78.
[22] K Ausubel, ibid. p.90
[23] NaturalNews.com: “American Medical Association Promoted Tobacco, Cigarettes in its Medical Journal,” http://www.facebook.com/note.php?note_id=44588419945
[24] Ibid.
[25] K Ausubel, ibid. p. 90
[27] Friedman, Milton; Rose D. Friedman (1990). Free to Choose: A Personal Statement. Mariner Books. pp. 240
[28] Mayer, ibid.
[29] G McAndrews, “Plaintiffs’ Summary of Proofs as an Aid to the Court,” Civil Action No. 76 C 3777, Wilk, (June 25, 1987) Throckmorton, Howard, Taylor, and Monaghon Deps.
[30] Bigos et al. US Dept. of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research, Clinical Practice Guideline, Number 14: Acute Low Back Problems in Adults AHCPR Publication No. 95-0642, (December 1994)
[31] Freeman MD and Mayer JM, NASS Contemporary Concepts in Spine Care: Spinal Manipulation Therapy For Acute Low Back Pain, The Spine Journal 2010 October; 10 (10):918-940
[32] Chou R, et al., Diagnosis and Treatment of Low Back Pain: A Joint Clinical Practice Guideline from the American College of Physicians and the American Pain Society, Low Back Pain Guidelines Panel, Annals of Internal Medicine 2007 October 2; 147 (7):478-491
[33]Milliman Care Guidelines for Lumbar Fusions, Low Back Pain and Lumbar Spine Conditions—Referral Management, www.allmedmd.com
[34] MD Freeman and JM Mayer “NASS Contemporary Concepts in Spine Care: Spinal Manipulation Therapy For Acute Low Back Pain,” The Spine Journal 10/10 (October 2010):918-940
[35] S Bigos et al.
[36] Her Majesty’s Stationery Office in London in its Report of a Clinical Standards Advisory Group Committee on Back Pain (1994)
[37] P Manga and D Angus, “Enhanced Chiropractic Coverage Under OHIP As A Means Of Reducing Health Care Costs, Attaining Better Health Outcomes And Achieving Equitable Access To Select Health Services.” Working paper, University of Ottawa, 98-02.
[38] C Manniche et al. “Low-Back Pain: Frequency, Management And Prevention From An HDA Perspective,” Danish Health Technology Assessment 1/1 (1999)
[39] McMorland G, Suter E, Casha S, duPlessis SI, and Hurbert RJ, Manipulation or microdiskectomy for sciatica? A prospective randomized clinical study, JMPT, 2010 Oct 33(8):5776-584.
[40] RA Deyo, “Low -Back Pain,” Scientific American, (August 1998):49-53
[41] G Waddell and OB Allan, “A Historical Perspective On Low Back Pain And disability, “Acta Orthop Scand 60 (suppl 234), (1989)
[42] SD Boden, DO Davis, TS Dina, NJ Patronas, SW Wiesel, “Abnormal Magnetic-Resonance Scans of the Lumbar Spine in Asymptomatic Subjects: A Prospective Investigation,” J Bone Joint Surg Am. 72 (1990):403–408.
[43] MC Jensen, MN Brant-Zawadzki, N Obuchowski, MT Modic, D Malkasian, JS Ross, “Magnetic Resonance Imaging Of The Lumbar Spine In People Without Back Pain,” N Engl J Med. 331 (1994):69–73.
[44] M Brandt, Stanford University Medical Center, “MRI Abundance May Lead To Excess In Back Surgery,” (Oct. 14, 2009)
[45] JD Baras and LC Baker, “Magnetic Resonance Imaging And Low Back Pain Care For Medicare Patients,” Health Aff (Millwood) 28/6 (2009):1133–40.
[46] RA Deyo and DL Patrick, Hope or Hype: The Obsession with Medical Advances and the High Cost of False Promises (2002):191.
[47] Deyo and Patrick, ibid.
[48] JN Weinstein et al., “Surgical vs. Nonoperative Treatment For Lumbar Disc Herniation: The Spine Patient Outcomes Research Trial (SPORT) Observational Cohort,” Journal of the American Medical Association 296 (2006):2451–9.
[49] A Dembner, “Spine Tuning, Innovative Surgeries Raise Hope, Concern,” Boston Globe Staff (September 3, 2007).
[50] “Spike in Complex Spinal Surgery Sets Off a Wave of Serious Complications and Exorbitant Costs,” The BACKLETTER, 25/6 (June 2010):61,67
[51] EJ Carragee, “The Increasing Morbidity of Elective Spinal Stenosis Surgery: Is It Necessary?” JAMA 303 (2010):1309-10
[52] B Graz, V Wietlisbach, F Porchet, JP Vader, “Prognosis or “Curabo Effect?”: Physician Prediction and Patient Outcome of Surgery for Low Back Pain and Sciatica,” Spine 30/12 (June 15, 2005):1448-1452
[53] G Waddell and OB Allan, “A Historical Perspective On Low Back Pain And Disability, “Acta Orthop Scand 60 (suppl 234), (1989)
[54] The BACKLETTER, 12/7 (July 2004):79
[55] The BACKPage editorial, The BACKLETTER, 20/7 (March 2005):84
[56] T Parker-Pope, “Americans Spend More to Treat Spine Woes,” New York Times (February 13, 2008).
[57] http://www.bcbsnc.com/assets/services/public/pdfs/medicalpolicy/lumbar_spine_fusion_surgery.pdf