Let me give you the chiropractic model of spinal care and overall health from a classical chiropractor’s perspective. Rather than looking at the outside of the spine—the joints, discs, and muscles—let us look at what happens inside the spinal column to the nerve system.
Indeed, this may be the first time you’ve ever been told the complex scientific basis behind chiropractic care, even for those who have seen a chiropractor. It has been the bane of this profession that many chiropractors treat or they speak in philosophical terms, but they don’t teach the logic and science of chiropractic care. Too often I’ve heard patients say “I believe in chiropractic,” but it is more important for them to understand it.
Just as medicine’s model of disease has evolved from bad spirits to germs to genetics, so too has chiropractic model of disease and health changed over the last century. Indeed, today’s chiropractic is not what your grandfather knew, nor is it what DD Palmer tried to explain.
The Madness to our Method
If you were to ask generally what most chiropractors do, the typical response would be simply, “They crack bones to help back pain and pinched nerves,” which makes me cringe in pain when I hear that so let me rephrase it: while we don’t crack bones, we do adjust spinal joints to alleviate pain and other neurological disorders that may accompany an injured or malfunctioning spine.
Obviously there’s more to our science than popping joints, but that’s a good place to begin; indeed, why do chiropractors focus on the spine to correct subluxations and why do most chiropractors not talk about health or disease solely as a function of germs or blood chemistry—the typical medical explanation for disease? These are essential differences to understand.
Chiropractic is a school of thought and not merely a treatment method. It is a method of analyzing health and disease from the perspective of your spine and nerve system rather than your blood as the medical profession primarily does. But don’t fall into the allopathic trap and think there is a specific adjustment for a particular problem as the medical profession offers a specific drug for an illness.
Virgil V. Strang, DC, longtime instructor and past president of Palmer College of Chiropractic, explained the philosophy behind the chiropractic method:
Nobody in his right mind claims to have the cure for any ailment. Nothing is a certainly in the health care field. Furthermore, nothing could be more misleading than to talk or write about chiropractic as though it were capable of being targeted at specific diseases. It is wrong to suggest directly or indirectly to patients that here is a headache adjustment, a diarrhea adjustment or a menstrual cramp adjustment. Often what results in a correction for one patient, requires a different approach for the next. Chiropractic does not stimulate or suppress the nervous system as does medicine. Chiropractic normalizes the nervous system. (emphasis added)
To do this, the chiropractor must consider much more than the symptoms; the chiropractors must consider what biomechanical problem is involved in causing or perpetuating the problem. Since any of several reflex patterns can cause a particular symptom, variety of biomechanical problems must be considered in any given case. While we can readily identify the final common pathway that is contributing to the dysfunction, we cannot with certainty surmise the reflex route that is the source of the problem.
So what can a chiropractor honestly say or write about the services offered to patients? First, it can be said that the chiropractor seeks to normalize the nervous system by finding and removing subluxations that are disturbing neurophysiological function. Second, it can be noted that patients frequently report that after receiving chiropractor care for a subluxation, various symptoms diminish or disappear. Third it can be related that some of the more common symptoms which historically have brought patients to chiropractors offices include: pain (neck, back, arm, hand, leg), numbness, burning and tingling (arm, hand, leg), headaches, menstrual cramps, abnormal length of menstrual cycle, gastritis, diarrhea, constipation, bed wetting, hypertension, nervousness, asthma, and vertigo. Fourth, chiropractic is not a panacea; therefore, in some cases patients will be referred to appropriate specialists.
Whether it is in conversations with new patients, in brochures in the office literature rack, in public lectures, or in mass media advertising, the chiropractor should avoid giving the impression that the adjustment corrects the disease. In truth, the adjustment corrects the subluxation. While this may clear the way for the nervous system and the associated homeostatic processes to restore health, the adjustment does not have a direct relation to the banishment of a disease. To be forthright on this matter dos not weaken the case for the chiropractic adjustment. In fact, it calls attention to the broad attributes of the adjustment. The adjustment, by normalizing the body’s nervous system, restores coordination to the body’s far-reaching system of homeostasis.[1]
Obviously there is a huge night-to-day difference in the philosophies of medicine and chiropractic. As DD Palmer wrote, “Chiropractic is not a branch of medicine. There is no more resemblance between Chiropractic and medicine than there is between a Chiropractor’s office and a drug store.”[2]
Not only is there a different medium, for example, blood versus nerves, but there is a different outlook on the entire healing process as Dr. Strang explains.
Let me begin this discussion on the madness to our method by stating there are different levels of healing that chiropractors focus upon—the physical and mechanical problems of the spine; the neuromusculoskeletal issues that cause problems like sciatica, radiating arm pain, and headaches; the spinal reflex and neuro-chemical aspects that remain only partially explainable by today’s science, and the intangible issues like wellness, vim, vigor, and vitality that are virtually unexplainable.
With a bad back, you can negatively affect all of these attributes and, indeed, only people with a strong backbone will have the benefits of all attributes of well-being. Remarkably, it is a factor of health and wellness that is constantly overlooked by the medical profession and the media.
For example, in the February, 2010, issue of Woman’s Day magazine, an article titled “142 Ways to Be Healthier,” failed to include one mention of a strong spine and a healthy, functioning nerve system, although this article did mention other healthy habits like nutrition and exercise; as well, it revealed a pharmaceutical bias with ten advertisements on medications, including one for Seroquel XR® with four pages consisting of fine print about the many dangerous side-effects. Apparently the hidden message here is you cannot be well without drugs.
Most people think of chiropractors as non-drug, non-surgical back doctors who treat only mechanical spinal problems for neck and back pain—the Type M disorders mentioned in the New Zealand Report. This is the acceptable musculoskeletal role in mainstream medicine that chiropractors fill without too much controversy nowadays. As you’ve learned by now, the researchers understands that spinal manipulative therapy and other hands-on therapies used by DCs are very effective for most spinal problems, just as the public understands chiropractors are effective as reported in the May 2009 article in the Consumer Reports magazine.[3]
Only a diehard medical chauvinist like NM Hadler would still argue that chiropractic doesn’t work for the majority of mechanical back pain problems, but these people remain in denial and mired in medical bigotry. Hopefully that generation of MDs is fading from the profession and taking their prejudicial attitudes with them. Few unbiased and informed MDs today would criticize chiropractors as specialists in non-drug, non-surgical spine specialists.
The glut of research today is just too high now to dispute the effectiveness of chiropractic care for the vast majority of spine problems, especially the majority of mechanical ones. Only a fool today would bash chiropractors with unfounded claims or try to scare patients with the voodoo diagnosis, telling them that chiropractic care is dangerous or placebo.
The remaining controversy still prevails over the Type O organic disorders that may respond to chiropractic as the New Zealand Report, Dr. Strang, and others scientists have mentioned. Indeed, most people are totally unaware that spinal subluxations are now linked to high blood pressure, angina, fibromyalgia, and even degeneration of the brain.
More remarkable is the fact this research has been done by PhDs and medical people, not by chiropractors. As the New Zealand investigators might have concluded, finally research is catching up to explain the chiropractic paradigm of health.
What people still don’t understand is why we adjust the spine instead of prescribing drugs, injecting shots or doing surgery—the standard medical methods. A short lesson in spinal anatomy will explain the why.
Although the nerve system is described by some as the master electrical system of the body controlling all other systems in conjunction with the endocrine system, it is probably the least understood part of the body by the public. Most people today are well versed in terms concerning the heart and circulatory system like cholesterol, triglycerides, and blood pressure, but painfully few understand how the nerve system works or how it can adversely affect your body by spinal injuries.
Terms like joint dysfunction, spinovisceral reflex, dysautonomia, and neurotransmitters and even the classic chiropractic term vertebral subluxation remain unfamiliar to the public. Despite being called the Master System, it should be called the Mystery System since the importance of the spine and the nerve system remains a mystery to most people.
A good example of this lack of understanding occurred when actor Christopher Reeve, who starred in Superman: The Movie, was severely injured in 1995 in a equestrian cross country event when his horse had a refusal and he was thrown off, causing a cervical spinal injury that paralyzed him from the neck down.[4]
During the Today Show with Katie Couric the next week, she asked a NYU neurosurgeon about this case, who showed with a plastic spine where Reeve’s spine was fractured—at the top two vertebrae, known as the Atlas/Axis—and the area of the spinal fusion.
“If he only broke those bones, why can’t he breathe and why is he paralyzed?” Katie asked the doctor. This opened the door to neurophysiology and how the spinal column affects the nerve system that, in turn, affects organ function.
The doctor explained how the nerves from the upper neck area—the brain stem—innervate and control major organ function, specifically in this case, the nerves to Reeve’s heart and lungs, necessitating the use of a breathing machine to keep him alive.
What the neurosurgeon said was true, but it made me realize the double standard in medicine. If I had said the same thing—that nerve compression in the brain steam due to vertebral misalignment might cause organic problems—the political medicine would have come down on me like a load of bricks for suggesting a link between the spine and Type O dysfunction.
Morris Fishbein, the Medical Mussolini who began the medical war against chiropractors in 1924, would be screaming from his grave, “Quackery!” but when a neurosurgeon from NYU says virtually the same thing, it is well-received as wisdom from a learned medical man.
Obviously in Reeve’s case, spinal manipulation was out of the question for his fractured neck, but I contend that if he fell hard enough to break his neck, undoubtedly he also compressed and misaligned probably every joint in his spine and body, and these areas could be helped greatly by gentle, specific spinal manipulation; certainly sitting in a wheelchair only added to the compression in his low and mid-back areas.
Perhaps Reeve’s lasting legacy will be from the aftermath of his accident. Until his death in 2004, Reeve lobbied for expanded federal funding on embryonic stem cell research to include all embryonic stem cell lines in existence and for open-ended scientific inquiry.[5] Before he finally passed away, Christopher became the Superman spokesman for every spinal cord injured person in America.
The Controversial Big Idea of Chiropractic
The single largest issue that remains subject to controversy between the medical and chiropractic communities is the scope of clinical effectiveness of chiropractors with non-back pain problems—the Type O disorders as the New Zealand Report mentioned occurred in 7 percent of Type M patients who visited chiropractors.
I daresay if all Type O patients were given access to chiropractic spinal care, this 7 percent may be higher considering the majority of patients with organic disorders are not treated by chiropractors concurrently with medical care.
Without question, the biggest objection by MDs toward chiropractors stems from the notion that chiropractic care helps patients in many Type O situations, not just for Type M—neck, back pain, and headaches—the common ailments patients seek help from chiropractors who often saw anecdotal cases of organic dysfunction improve in their offices, but science then was unable to explain the how and why.
The treatment by manipulation of Type O disorders not related to Type M disorders has been supported by clinical experience and case reports according to William Meeker, DC, MPH, and Scott Haldeman, DC PhD, MD, FRCP(C).[6] These include randomized clinical trials for primary dysmenorrhea[7],[8], hypertension[9],[10], chronic asthma[11],[12], enuresis[13], infantile colic[14], and premenstrual syndrome[15], which have been completed with varied results.
Certainly the real controversy pits those who understand and accept anatomical issues like joint dysfunction to help neck and back pain, and the other camp that cannot understand how the same anatomical issues in the spine and musculoskeletal system may affect physiologic regulation and function as well.
Indeed, the Big Idea of chiropractic suggests the actual scope of chiropractic is as vast as the nerve system itself. The original iconic chiropractors—the Palmer father and son, DD and BJ Palmer—were not interested in low back pain or whiplash—the typical musculoskeletal disorders that chiropractors commonly treat so successfully.
Instead, the Palmers were interested in the function of the body’s organs and overall homeostasis via the nerve system. They were, in effect, among the earliest neuroscientists who lectured on the affect of spinal dysfunction on neurophysiology caused by interference to the nerve system via mechanical distortions in the spine. Although a mouthful, it is that simple.
Andrew T. Still, the founder of osteopathy, also taught the value of the physiological benefits of treating “spinal lesions,” his synonym for DD Palmer’s “vertebral subluxation.” For example, as far back as 1899, C. Hazzard, an osteopathic physician, wrote of this duality of treatment for either structural problems or functional issues.
“In our treatment of the spine there are two points which we may take into consideration…In the first place we may wish to treat the spine itself. In the second place, we may wish to reach, by treating the centers along the spine, the viscera to which these nerves run. It is not always possible to disassociate these in your practice.”[16]
The problem with the concept of neurophysiologic regulation through manual therapy was that it was ahead of its time. You have to remember that at the first turn of the 20th century, America was still in the horse and buggy era, and so was medical science.
Research could not explain the belief that the central nerve system controlled function, and thus, interference to the nerve system created “dis-ease” as the Palmers described the change in homeostasis, but this “dis-ease” had nothing to do to germs; it had to do with spinal joint dysfunction causing nerve-related health problems.
Consequently, the Palmers resorted to what is now considered rather crude scientific terms and metaphysical concepts to explain the neurological component of chronic diseases. They spoke in terms of “innate intelligence” and other vitalistic terms to describe the mechanisms of nerve dysfunction. To this day, some fundamentalist advocates still preach this metaphysical bio-theosophy as chiropractic’s sine qua non according to historian Joseph Keating, PhD.[17]
“Chiropractors have gained some credibility in recent years as providers of quality health care services for patients with disorders of the musculoskeletal system. However, the chiropractic profession has long been and continues to be ridiculed for advocating the broader clinical utility of manipulative procedures, for example, for patients with cancer, diseases of the viscera, cardiovascular disorders and psychiatric conditions. The persistence of these broader claims despite the absence of scientific evidence is partly attributable to dogmatic adherence to rigid, unchanging, and largely unchallenged theories of disease causation (e.g., subluxation) and intervention. Indeed, some chiropractors take pride in the supposedly unchanging character of chiropractic paradigms.”[18]
Rather than the “unchanging character of chiropractic paradigms,” I would suggest it as an evolving paradigm. Although chiropractors saw the impact of spinal adjustments upon patients’ health, they attempted to explain this in terms that were used by healers at the turn of the late 1890s and early 1900s.
DD Palmer, the founder of the chiropractic profession, in 1910 wrote on the title page of his book, The Chiropractor’s Adjustor, that the main principle of chiropractic was “Founded on Tone.”
It was Palmer’s contention that too much or too little tone will create a state of inflammation in tissues and altered function, a legitimate concept still today, but one he resorted to vitalistic terms to explain.
“Life is the expression of tone. In that sentence is the basic principle of Chiropractic. Tone is the normal degree of nerve tension. Tone is expressed in functions by normal elasticity, activity, strength and excitability of the various organs, as observed in the state of health. Consequently, the cause of dis-ease is any variation of tone—nerves too tense or too slack.
“The nerve system is the channel thru and by which life-force—the energy which gives innervation to the essential functions of respiration and circulation—is transmitted. The two latter are the functions upon which life depends. They are carried on in proportion to the innervating force which, as we have noticed, may be either excessive or deficient, either condition causing disease and even death.
“The involuntary portion of the nerve system and muscles which contract by nerve stimuli must be in normal tone in order to execute the normal amount of functionating for a health existence.
“Excessive tonicity causes erethism, an abnormal increase of nerve irritability, an augmentation of vital phenomena in organs or tissue. Deficient tonicity causes atony or weakness, a lack of vitality.
“Tone is a term used to denote a normal degree of vigor, tension, activity, strength and excitability of nerves and muscles, as observed in a state of health—the effect of tonicity. Tonicity determines the tone. Excessive tonicity causes an augmentation of vital phenomena; a deficiency of tonicity, a want of tone, a loss or diminution of muscular or vital strength.”[19]
According to historian Joseph Keating, at this early stage of chiropractic in the period from 1897 through 1902, DD Palmer believed that displaced anatomy is the cause of inflammation and disease. By the 1908-10 period Palmer seemed to think of the nerves as a meshwork stretched over the bony framework of the body; the normal tension of the nerves was determined by the proper alignment of the skeleton. Palmer had come to believe that subluxations usually produced an increase in nerve tension, thereby accelerating mental (vibrational) impulses to end organs, which resulted in increased “molecular vibrations,” friction, heat and inflammation. In this respect, Palmer’s 1910 chiropractic had retained much of his original theory: “as ever, chiropractic was predominantly a theory of inflammation.” [20]
Palmer’s notion of ‘tone’ provides a theoretical bridge between his concepts of vital (Innate) force and dis-ease in the body via subluxations. Tone, the neurally-mediated health of individual cells and body parts, was construed to originate in the life force known as Innate Intelligence, and to be disrupted by impingement upon nerves. Such impingements, rather than obstructing nerve flow (as in BJ’s “nerve-pinching” notions), caused an increase or a slackening of tension in the nerve, thereby altering the vibrational rate of impulse transmission.
Ironically, much that is potentially testable in Palmer’s theories has been forgotten by chiropractors who focus on musculoskeletal disorders. As well, after DD’s death in 1913, BJ Palmer’s simplistic metaphor of “pressure on the hose” had replaced DD Palmer’s belief in vibrational nerve transmission, aggravated nerve tension, and altered tone. This was a backwards step in the evolution of chiropractic science.
Many if not most chiropractors today remain unaware that D.D. Palmer’s chiropractic theory of inflammation, which also has been validated as a contributor to many chronic illnesses such as stroke and arthritis. In fact, nearly 100 years afterwards, medical researchers now contend that inflammation is worse for the heart than cholesterol.[21]
According to Keating, “Whether or not Palmer’s theories would stand up in light of present day knowledge of neuroanatomy and physiology remains to be seen.”19
Modern Neurophysiology
It may have taken nearly a century for science to catch up to chiropractic’s claims, but many modern neurophysiologists now support the basis of the role of the spine upon the homeostasis of the body. The New Zealand Report heard testimony from such neurophysiologists and had the foresight to realize chiropractic science was very limited in its understanding of the madness behind its methods, but researchers like Irvin M. Korr, PhD, from Princeton University and Virgil V. Strang, DC, HCD, from Palmer College of Chiropractic, among many, have championed this concept.
Not only did these modern researchers elaborate on the neurophysiology of the vertebral subluxation, they also proposed a paradigm shift in the basic perspective we ought to have in considering health. In other words, rather than the allopathic medical concepts of the germ theory and the importance of organs, Korr eschewed the medical approach of glorifying the viscera which, he believed, are merely specialized muscles designed to maintain the musculoskeletal system.[22]
Korr believed medical profession misunderstood the true nature of the human being, according to Craig Liebenson, DC.
“For Korr, what made us human was our ability to ‘will action’. We express our humanness by choosing to play piano, ski, etc. This concept anchored the osteopathic field in the ennobling area of taking care of the ‘whole’ person, while allopathic physicians were more reductionists.”[23]
Chiropractors like Virgil Strang[24] might take Korr’s paradigm one step further by suggesting neither the organs or muscles are paramount; in fact, those organs, muscles, and bones simply work together to convert food, water, and air into energy to maintain homeostasis in the body in order to move about the brain and nerve system. We are, indeed, mobile brain animals first and foremost; consequently, any damage to this nerve system via spinal subluxations may manifest as organic disease and muscular disorders.
According to Strang, “chiropractic’s rationale begins with the law of biology known as homeostasis.”[25] Gray’s Anatomy defines homeostasis as:
Such a preservation of internal constancy, or homeostasis, despite short-term fluctuations in the surroundings, is a central feature of the operation of all the principle organ systems, for example, the regulation of temperature, blood pressure, hydration, osmolarity, electrolyte and hydrogen ion concentrations, glucose and oxygen levels, etc.[26]
Dr. Strang believes the importance on homeostasis is the key difference between chiropractic’s paradigm and the medical mindset.
Because homeostasis is essentially a system of mechanisms responding to negative feedback, chiropractors begin their diagnosis of patients with this classic chiropractic question: “What has happened to the homeostatic system?” Notice, the question is not, “What has happened to homeostasis?” Nor is the question “What has happened to the dysfunctioning organ?” – although this may well be asked subsequently. The initial question which characterizes the chiropractic approach to patient care is, “What has happened to the homeostatic system?” i.e., “What has happened to the sensory, integrative, and effector coordinates upon which homeostasis depends?”[27]
Korr also mentioned the role of homeostasis that allows the nerve system to control the tissues of the body to its every changing environment. He found damage or interference primarily at the spine, which he referred to as ectopic impulses, would cause “cross-talk” of meaningless commands by joining the real commands with gibberish causing uncoordinated motor and autonomic responses. In turn, this might cause disruption in the function of organs and muscles; therefore, therapy like spinal adjustments to correct vertebral subluxations directed at silencing or reducing this “gibberish” traffic in the affected sympathetic pathways is often ameliorative.[28]
The early chiropractic principle suggests that chiropractic consists of normal transmission of ‘mental impulses’ was not too distant from Korr’s concept of gibberish. DD Palmer wrote that “In disease, mental impulses are not impeded, hindered, stopped or cut off – they are modified. An impingement does not obstruct; it is either an excitor or a depressor.”[29] While this explanation of neurophysiology may be crude by today’s standards, it wasn’t entirely incorrect either.
Korr also found that the effects of insult on nerves affected the trophic influences of those neurons by altering the neuro-chemicals that flow along the nerves themselves. Although most people understand the concept of “atrophy” as the process of degeneration or dying, the concept of “trophism” is the life-sustaining aspect of the nerve system, such as nourishment.
Korr demonstrated mechanical derangement of axoplasmic flow in rabbits and noted the following:
“Deformations of nerves and roots, such as compression, stretching, angulation, and torsion that are known to occur all too commonly in the human being […] are subject to manipulative amelioration and correction.” [30]
The founder of osteopathy, Andrew Still[31] also alluded to axoplasmic flow and attributed the cause of dysfunction to “partial or complete failure of the nerves to properly conduct the fluids of life.”
Dr. Korr’s research in the 1960-70s focused on this new concept in neuro-physiology called trophic functions of nerves. He and his associates produced exciting work revealing that nerves not only conduct bio-electrical impulses to muscles, but also supply chemical nourishment to organs through continuous transfer of proteins and other substances along the nerve fibers. This research demonstrated that nerve compression may interrupt or reduce the ‘axoplasmic flow’ of material from nerve to muscle, influencing muscle structure, excitability, contractile properties and metabolism. Korr postulated that one mechanism by which spinal manipulation achieves its affects may be by removing this obstruction to trophic function in compromised nerves.[32]
Research by H.T. Vernon, DC, and M.S. Dhami, PhD, perhaps best summarizes the impact of the effects of spinal adjustments upon the whole body:
“There is now good evidence that spinal adjustment decreases pain, increases range of movement, increases pain tolerance in the skin and deeper muscle structures, raises beta-endorphin levels in the blood plasma and… has potent impact on a variety of nerve pathways between the soma and viscera that regulate good health.”[33]
I find it saddening that Americans have become so myopic about their health analysis, depending solely upon blood analysis as the guiding factor in their diagnosis. I mention to my patients to use their car problems as an analogy: If a car doesn’t start, what’s the first thing they would check? Would they first change their oil, their gas, the water in their engines or simply add STP to the crankcase? Probably not, because most people would check their battery and electrical system first if their car didn’t start or suddenly stopped.
But when it comes to our body’s health, rarely do patients have their spines checked to see if nerve interference may be the reason why their organs don’t work well or prematurely die. Although international research is replete with such neurological explanations, few people are told of this co-factor of organic disease. Indeed, if the electronics industry were controlled by political medicine, it would still be in the vacuum tube era. Ironically, while modern medicine utilizes many high-tech instruments, much of their basic philosophy remains in the last century.
Not only do organs require proper blood flow to function, but proper nerve function also is required to sustain the organs. But few people understand that even the essential blood flow is also controlled by the nerve system and, thus, any interference in these regulating nerves can cause blood circulation problems. Once again, let H.T. Vernon, DC, explain this physiological fact:
Every function in the human body, be it conscious or otherwise, depends upon nerve energy. This energy has its source in the cells of the brain and spinal cord. Even the caliber of the blood vessels throughout the entire body is under the control of the nervous system. The blood aspect of disease permits the use of an interesting illustration which applies to many other disease processes.
For example, if the nerves supplying the blood vessels are disturbed, then normal generation, transmission, distribution, or expression of the nerve energy is interfered with, and the vessels become either contracted or dilated as the case may be. This contraction or dilation prevents normal blood circulation, and this insufficient or excessive blood supply, technically known as ischemia or hyperemia, may cause the organ which it supplies to become diseased.
It should be understood that this is merely one of the many possibilities of nerve disturbance: What applies to this, likewise applies to all the nerves that regulate the ductless glands, the digestive and respiratory systems, and every other tissue, gland, organ, and system in the body. Interference with the nerve supply may cause disease in any of these tissues, glands, organs, and systems.[34]
As proof in point, in December 1989 an enlightening article appeared in the Journal of Manipulative and Physiological Therapeutics by Mark E. Jarmel, DC, titled “Possible Role of Spinal Joint Dysfunction in the Genesis of Sudden Cardiac Death.”[35] He noted that sudden cardiac death causes about 15% of all natural fatalities in the industrially developed countries. In the United States alone, it claims over 400,000 lives each year. Anecdotal reports from the chiropractic and osteopathic professions have indicated the beneficial effects of manipulation in the management of arrhythmias, coronary arterial spasm, and premature ventricular contractions. Dr. Jarmel’s study simply suggests that nerve irritation from the spine will cause heart problems:
“Numerous researchers have concluded that strategies for prevention of sudden death should be focused on controlling neurophysiologic factors which may enhance ventricular vulnerability. By removing a source of destabilizing neural input to the heart, correction of vertebral dysfunction may prove of value in reducing susceptibility to sudden cardiac arrest.”
Explaining organ function, dysfunction or failure as a result of vertebral subluxation is unfamiliar for most people. Few people ever think of heart disease in terms of dysfunction of their nerve system. Instead, they focus on other contributors such as smoking, lack of exercise, junk phoods and the “bad blood” nutritional concepts like cholesterol levels. Even being physically fit and eating correctly may not be assurance enough to avoid a sudden heart attack, as evident in the sudden deaths of basketball players such as Hank Gathers from Loyola-Marymount in Los Angeles, “Pistol Pete” Maravich, the former NBA All-Pro, and Reggie Lewis of the Boston Celtics.
Dr. Jarmel noted in his study of 79 cases of sudden cardiac death in people 18-35 years of age, three of them were competitive athletes. “This may suggest,” according to Jarmel, “that so-called ‘physical fitness’ may provide little cardiovascular protection when asymptomatic coronary artery disease is combined with neurally induced vasomotor disturbance.” In my mind, it’s equivalent to a race car with a big engine that fails because of faulty electrical wiring although nothing is mechanically wrong with the engine itself.
Dr. Jarmel’s main premise that nerve irritation may lead to a sudden heart attack and that spinal adjustments may help alleviate or prevent such problems should come as no surprise to any chiropractor or researcher with an understanding of neuro-anatomy and spinal mechanics.
Along the same concept by Korr concerning ectopic gibberish, another article by Mark Jarmel, DC, along with Judith Zatkin, Ph.D., of Cleveland College of Chiropractic in L.A. titled “Improvement of Cardiac Autonomic Regulation Following Spinal Manipulative Therapy” suggests the magnitude of this problem.
Their paper mentioned a trial about heart conditions and chiropractic care, which may substantiate the claim of vertebral subluxations as a plausible explanation of sudden heart attacks.
Unbalanced activation of cardiac sympathetic nerves plays a crucial role in the pathogenesis of sudden cardiac death. It has been proposed that mechanical irritation of upper thoracic vertebral joints may create an ectopic source of unbalanced cardiac sympathetic nerve activation. Spinal manipulative therapy is hypothesized to modulate mechanically induced sympathetic activity by restoring proper mobility to dysfunctional vertebral joints. This study evaluated the possibility that spinal manipulative therapy may have value in treating a previously unrecognized source of unbalanced cardiac autonomic regulation.
Eleven patients without a prior history of myocardial infarction who were found to have signs of dysrhythmic abnormalities on Holter monitoring, received a one month course of chiropractic manipulative treatment. After one month of spinal manipulative therapy, follow-up 24 hour ECG recordings were performed. A positive trend was noted in the number of ventricular beats, number of ischemic events, maximum time of ST segment depression, elimination of after-depolarizations, and enhanced heart rate variability. These preliminary results suggest that spinal manipulative therapy may significantly enhance cardiac autonomic balance.
The results of this study suggest that upper thoracic spinal joint dysfunction may be a previously unrecognized source of cardiac sympathetic activation. The results of this study may have implications for developing a novel nonpharmacological treatment which may have value in reducing risk of sudden cardiac death.[36]
Sympathetic vs. Parasympathetic Balance = Tone
A simple lesson in neuroanatomy may be helpful to the uninitiated at this point to understand Palmer’s concept of Tone as well as the homeostasis concepts discussed by Korr, Jarmel, and Strang.
The central nerve system (CNS) is that part of the nerve system that consists of the brain and spinal cord. The CNS is one of the two major divisions of the nerve system. The other is the peripheral nerve system (PNS) which is outside the brain and spinal cord.
The PNS connects the CNS to sensory organs such as the eye and ear, other organs of the body, muscles, blood vessels and glands. The peripheral nerves include the 12 cranial nerves, the spinal nerves and roots, and what are called the autonomic nerves that are concerned specifically with the regulation of the heart muscle, the muscles in blood vessel walls, and glands.
The autonomic nerve system (ANS) or visceral nerve system is the part of the PNS that acts as a control system, maintaining homeostasis in the body. These activities are generally performed without conscious control.[37]
The ANS controls the “unconscious” bodily functions, such as heart rate, digestion, and breathing patterns and consists of two parts: the sympathetic system and the parasympathetic system.
The sympathetic system can best be thought of as controlling the “fight or flight” reactions of the body, producing the rapid heart rates, increased breathing, and increased blood flow to the muscles that are necessary when an individual is in danger or under stress. This division also causes palms to sweat, pupils to dilate, and hair to stand on end. It slows body processes that are less important in emergencies, such as digestion and urination.
The parasympathetic system controls the “quiet” body functions, for instance, the digestive system, and is responsible for the “rest and digest” aspects of your health. The parasympathetic division controls body process during ordinary situations. Generally, it conserves and restores, slows the heart rate and decreases blood pressure. It stimulates the gastrointestinal tract to process food and eliminates waste.
In short, the sympathetic system gets the body ready for action, while the parasympathetic system gets the body ready for rest. And in normal individuals, the parasympathetic and sympathetic components of the autonomic nerve systems are in perfect balance, from moment to moment, depending on the body’s instantaneous needs.[38]
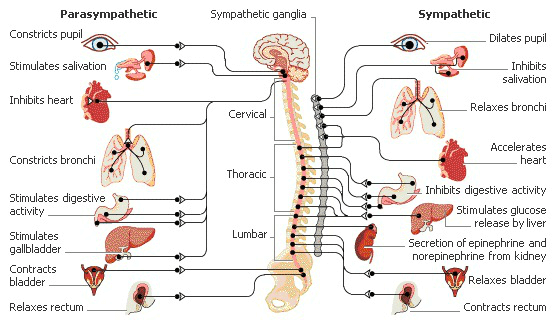
Balance between parasympathetic and sympathetic creates “tone” controlled by the hypothalamus located in the brain.[40] The hypothalamus regulates homeostasis and areas for thirst, hunger, body temperature, water balance, and blood pressure, and links the nerve system to the endocrine system.
Sometimes the two divisions have opposite effects on the same organ. For example, the sympathetic division increases blood pressure, and the parasympathetic division decreases it. Overall, the two divisions work together to ensure that the body responds appropriately to different situations by changing the tone of the organs.
In fact, a pilot study by George L. Bakris, MD, et al. has shown that “anatomical abnormalities of the cervical spine at the level of the Atlas vertebra are associated with relative ischemia of the brainstem circulation and increased blood pressure (BP). Manual correction of this mal-alignment has been associated with reduced arterial pressure.”[41]
The authors concluded that restoration of Atlas alignment is associated with marked and sustained reductions in BP similar to the use of two-drug combination therapy.
Often the sympathetic and parasympathetic divisions pull in different directions. When the sympathetic tone goes up, the parasympathetic tone goes down, and visa versa. Sympathetic stimulation, for example, opens the eye’s iris so you can see the intruder at the door, and it stimulated the heart rate so you can run from it or fight it. Parasympathetic stimulation will on the contrary narrow the iris and slow the heart beat to allow for rest and repair.
The point of varying the degree of tone from taught to flaccid is to change the organ response to the environment—whether to fight-flight or rest-digest.
A healthy ANS responds fluidly to changes and stressors in the environment and easily maintains homeostasis, both in our inner and outer worlds, and between our bodies and minds.
The chiropractic premise is simple: if the ANS has nerve interference due to spinal dysfunction affects the balance between the sympathetic and parasympathetic systems, hence a change of tissue tone may change the function of the organ or muscle, leading to a state of “dis-ease” as Palmer noted. This change has nothing to do with germs or genetics, but it is an imbalance of the ANS to alter the tone of tissue, hence, the functioning of organs and muscles.
Dysautonomia: New Term for an Old Condition
Dysautonomia literally means dysregulation of the autonomic nervous system. Dysregulation of the autonomic nervous system can produce the apparent malfunction of the organs it regulates. For this reason, dysautonomia patients often present with numerous, seemingly unrelated maladies.
In the 19th and early 20th centuries there used to be a condition called “neurasthenia.” People would find themselves suddenly unable to function, due to a host of inexplicable symptoms, often including fatigue, weakness, strange pains, dizziness, and passing out. Doctors would not find anything to explain these symptoms, so they were attributed to a “weak nervous system,” or neurasthenia.
According to Richard N. Fogoros, MD, most doctors hearing about this mysterious condition merely shake their heads in wonder. A century ago people would have been called neurasthenics today are given a host of diagnoses. These include chronic fatigue syndrome (CFS,) vasovagal or neurocardiogenic syncope, (which is a malaise mediated by the vagus nerve), panic attacks, anxiety, inappropriate sinus tachycardia, irritable bowel syndrome, postural orthostatic tachycardia syndrome, or fibromyalgia. Sufferers of all these conditions tend to experience an imbalance in the autonomic nervous system—an imbalance called “dysautonomia”.[42]
In people suffering from dysautonomia, the autonomic nervous system loses the normal balance, and at various times the parasympathetic or sympathetic systems inappropriately predominate. Symptoms can include frequent, vague but disturbing aches and pains, faintness (or even actual fainting spells), fatigue and inertia, severe anxiety attacks, tachycardia, hypotension, poor exercise tolerance, gastrointestinal symptoms such as irritable bowel syndrome, sweating, dizziness, blurred vision, numbness and tingling, anxiety and (quite understandably), depression.
The severity of the symptoms in people with dysautonomia are typically far out of proportion to any objective physical or laboratory findings (especially when the doctors don’t know which findings to look for). This lack of objective findings makes life very difficult. In modern medical practice, grounded as it is in the gathering and interpretation of objective data, when patients have the audacity to complain of symptoms without providing the objective medical findings like blood work to back them up, they are often written off as being hysterical.
Chiropractors hear this complaint a lot from patients who have had the medical drug treatments, but still complain of their aches, pains, and dysfunction or disability. Often these skeptical MDs simply cast them off as malingering or telling them “it’s all in your head.” In fact, they’re close: it’s all in their spines.
Whatever the diagnosis, however, a dysfunctional autonomic nervous system almost always plays a major part in causing the symptoms. And whatever the symptoms and whatever the diagnosis, all these syndromes are real, honest-to-goodness physiological (as opposed to psychological) disorders – probably variants of the same general disorder of the autonomic nervous system – and while “they can make anybody crazy, they are not caused by craziness,” according to Richard N. Fogoros, MD. [43]
Dysautonomia are caused by many different things, and do not have one, single, universal cause. Dysautonomias caused by viral infections, toxic exposures, or trauma often have a rather sudden onset. What is generally ignored is spinal trauma that may cause the imbalance between the sympathetic and parasympathetic nerve function, just as spinal care is often ignored as a treatment for fibromyalgia despite being recommended by the Academy of American Family Physicians.[44]
This explanation of the Autonomic Nerve System and the consequences of an imbalance between the two complimentary systems is not meant to be an academic lesson as much as a simple discussion how a chiropractic spinal adjustment may affect organ dysfunction as well as altered homeostasis—the condition ol’ DD Palmer simply called “dis-ease.” Recent research now offers another concept of neurophysiology that has gotten more attention.
A Modern Explanation: The Somatovisceral Reflex
Perhaps DD Palmer’s concept of inflammation being a response from “aggravated nerve tension and altered tone” was a concept ahead of its time for both the medical profession and public to understand. Even today, neurological disorders are difficult to understand compared to the simplicity of the germ theory where you “catch” disease rather than a neurological disorder that develops over time.
Through the decades of chiropractic practice, the single biggest bone of contention with some in the medical world who cannot understand how spinal manipulation helps organ problems. Again, they must forget that the nerve system is the key to this link, and it begins with a process known as somatovisceral reflex as neurophysiologists tell us.
This research may explain another connection between this phenomenon of neural healing via chiropractic spinal care. It may have taken over 100 years for science to understand this avenue of healing, but finally new theories are emerging with interesting explanations.
A survey of clinical studies found reports of various visceral symptoms being relieved by treatment of the spine.[45] In an attempt to justify the treatment of these conditions and numerous anecdotal reports of success with some of these conditions, chiropractors have sought to explain the mechanism of what they are doing by using well-established neurophysiologic explanations.
The original and rather archaic “pinched nerve” theory has been abandoned and replaced by the “reflex-based” theory. While this became a modern explanation, it too has been modified by recent investigators, such as . Nansel, Szlazak, Budgell, and Sato.[46]
The “somatovisceral reflex” is at the core of this explanation. Reflex effects have been demonstrated throughout the cardiovascular system, in the digestive system, urinary system, endocrine system and immune system.[47]
“Thus, this may be another potential explanation for the anecdotal success of Type O (organic) treatments reported by so many chiropractors. This explanation is not normally discussed as being a factor in the etiology or treatment of the Type O condition,” according to Dr. Henry Pollard who warns chiropractors about being too enthusiastic about treatment of these organic disorders. [48]
“Despite anecdotal claims of success with organic conditions, success in management is not guaranteed nor is it predictable. Treatment is at best a trial of therapy rather than a known quantity. Unfortunately, some practitioners are overzealous in their expectation of outcome, and this expectation is conveyed to the patient. Although such a positive expectation can be associated with its own positive outcomes, it is irresponsible to claim a certainty in outcome when none has been established…I propose that it is for these reasons that chiropractic treatment of the Type O condition is often questioned.” [49]
There is not as much awareness by MDs or the public that musculoskeletal problems including back pain, thoracic outlet syndrome, and myofascial syndrome can cause similar complaints like chest pains/angina, including an initial impression that the heart is the source when, in fact, it is not.
The somatovisceral or somatoautonomic reflex is thought to result from the stimulation of somatic structures (skin, muscle, ligament, bone, etc) to cause a reflex change in the efferent (out-going nerves) output to an organ. These spinal reflexes span the visceral organs and have been investigated by many researchers.
Somato means muscles, ligament, and joints; visceral pertains to internal organs. A reflex action, also known as a reflex, is an involuntary and nearly instantaneous movement in response to a stimulus, such as noxious chemicals or a spinal disorder in this case.
Somatic nerve stimulation can regulate various visceral functions by responses that are reflex in nature. One conclusion by Sato et al. emerging from the evidence presented is that the effects of somatic stimulation are dependent upon the particular organs and on the spinal segments. The analysis of neural mechanisms of these reflex responses seems to be very important for clinical application to regulate visceral function by physical treatment.[50]
For example, in anesthetized cats, Sato found that movement of the knee joint within its normal physiological range has no effect on blood pressure or heart rate. However, forced movement beyond the normal physiological range of motion produces significant increases in the heart rate and blood pressure. On the other hand, in the acutely inflamed joint, these responses are greatly exaggerated. In fact, in the inflamed joint, even movement within the normal range produces reflex increases in blood pressure and heart rate. Similar observations abound: noxious stimulation elicits clear and consistent autonomic responses; innocuous stimulation elicits weak and inconsistent responses or none at all. [51]
Recent neuroscience research supports a neurophysiologic rationale for the concept that abnormal stimulation of spinal or paraspinal (brain) structures may lead to reflex responses of the autonomic nerve system, which in turn may alter organ function.[52] In other words, a back injury can cause the nerves in that region of the spinal column to have a reflex reaction in the organs that are innervated by them. Muscle reflex spasms also occur when nerves in the spinal joints are injured.
Some patients with persistent abdominal, side, chest, or groin pain often remain undiagnosed after repeated doctor visits for a full blood workup fails to reveal a source of the organ system involved. Just as back pain patients who have had MRIs that show no disc abnormality are often misdiagnosed because joint dysfunction is overlooked, so too are patients with somatovisceral reflex problems misdiagnosed when the blood workup comes back normal. This only adds to their suffering with self-doubt and then depression may begin from not knowing if they have a serious undetected illness or not.
This is where a good chiropractic evaluation can help. For many, examination of the somatic system (muscles, nerves and ligaments) can hold the answer. Rather than being told by the family physician that “it’s all in your head,” he should tell you “It may be coming from your spine.”
Most of us understand that one sign of a heart attack is referral of pain into the chest wall and down the left arm. Many of my patients think they’re having a heart attack when this type of pain strikes them. They have the ECG and blood work only to be told everything is okay, but they remain in pain. I cannot tell you how many supposed heart attacks I have helped with a simple spinal adjustment that stops this reflex phenomenon.
Spinovisceral Reflexes
A study conducted by Sato and Swenson[53] investigated the effects of mechanical stimulation of the spine on blood pressure, heart rate and renal sympathetic nerve activity. New evidence suggests that muscle spindles in the neck muscles may in fact be capable of eliciting somatoautonomic reflexes.[54] Additionally, there is recent evidence from studies in humans that mild stimulation of the neck muscles may influence cardiovascular function.[55]
Nansel and Szlazak from Palmer College of Chiropractic-West in San Jose, California, did an in-depth study of somatovisceral theories of over 350 articles spanning the last 75 years and found that it has been firmly established that somatic dysfunction is notorious in its ability to create overt signs and symptoms that can mimic, or simulate rather than cause, internal organ disease. In fact, they believe as much as 10’% of supposed heart attacks may be caused by this syndrome.[56]
They added that “Unfortunately, these well-documented, ‘pseudo’ or ‘simulated’ visceral disease syndromes can often be responsible for a significant number of medical misdiagnoses…the existence of these somatic visceral disease mimicry syndromes obviously justifies a highly important mandate for increased cooperation between the medical physician and those who specialize in the evaluation and treatment of various aspects of primary somatic dysfunction.”
Indeed, David Seaman and James Winterstein now agree that spinal joint complex dysfunction should be included in the differential diagnosis of pain and visceral symptoms because “joint complex dysfunction can often generate symptoms which are similar to those produced by true visceral disease.”[57]
Neurotransmitters: Another Unknown Key to Health
In addition, those investigating the somatoautonomic reflexes point to the important role that the brain influences have on somatic and visceral structures of the body. These supraspinal centers refer to the combined action of higher brain centers such as the thalamus, reticular formation, cerebellum, cortex, hypothalamus, and limbic system.
Unlike the electrical system in your home that is dry, the human electrical system is wet with chemicals called neurotransmitters that influence the action of the nerve system which, in turn, affects the function of organs. Researchers now understand how the alterations of these neurotransmitters and hormones influence the functioning of your organs and your overall health.
Nerves secrete chemical substances called neurotransmitters that are endogenous chemicals which relay, amplify, and modulate signals between a neuron and another cell. Neurotransmitters are chemicals that are stored in nerve endings or terminals located in the brain. They are also found at the axon endings of motor neurons, where they stimulate the muscle fibers to contract. And they and their close relatives are produced by some glands such as the pituitary and the adrenal glands.
The brain controls the regulation of your body functions via these neurotransmitters that have different actions. The problem of some disorders begin when these hormones are out of control due to diet, lack of exercise, depletion of vitamins, stress, or spine injury, which is a relatively new concept.
Now another neurophysiologic factor has been found that may also influence your health, and this one may start in your back and end up in your brain.
In an article published in The Journal of Neuroscience, A. Vania Apkarian, PhD, et al. from Northwestern University has shown that long standing back pain may lead to altered neurotransmitters and serious brain degeneration. He found in MRI studies that chronic back pain can shrink the brain by as much as 11%, equivalent to the amount of gray matter lost in 10 to 20 years.[58]
Using magnetic resonance imaging brain scan data and automated analysis techniques, chronic back pain patients were divided into neuropathic, exhibiting pain because of sciatic nerve damage, and non-neuropathic groups.
“Patients with chronic back pain showed 5-11% less neocortical gray matter volume than control subjects. The magnitude of this decrease is equivalent to the gray matter volume lost in 10-20 years of normal aging. The decreased volume was related to pain duration, indicating a 1.3 cm3 loss of gray matter for every year of chronic pain…Our results imply that chronic back pain is accompanied by brain atrophy and suggest that the pathophysiology of chronic pain includes thalamocortical processes.”
In an interview, Dr. Apkarian said, “We basically studied 26 chronic back pain patients…and compared them to 26 normal subjects who had similar age and sex distribution. And we looked at the overall volume of the gray matter of the cortex. And essentially we find significant decrease in the overall volume of the brain gray matter in the back pain patients.” [59]
Apkarian says one of the areas of the brain impacted by chronic back pain is the prefrontal cortex. “The prefrontal cortex is important because it’s a region that has to do with cognition. It’s the highest area of the brain and has to do with a lot of decision making, rational thinking, and decisions along those lines. Obviously that’s an important area of the brain to become dysfunctional.”
Apkarian says he hopes his study causes those who suffer from chronic back pain to seek out solutions. “You should try to seek ways to reduce the pain, and that one should not live with the pain. The longer you live with the pain, the worse the impact on the brain. So one needs to actively find methods or therapies that would diminish the suffering as much as possible.”
Perhaps this study affirms the belief that a sequential pattern exists in the brain and nerve system: spinal injuries causing spinal cord stress causes neurotransmitter changes slowly leading to cerebral degeneration that then manifests itself as neurologic disorders.
In this light, chiropractic spinal adjustments that reduce or eliminate back pain would possibly reduce altered neurotransmitter changes that may cause damage to the brain and, thus, improve the brain circuitry of pain and dysfunction.
In yet another article in The Journal of Neuroscience by Marwan N. Baliki, et al., “Beyond Feeling: Chronic Pain Hurts the Brain, Disrupting the Default-Mode Network Dynamics,” these neuroscientists believe chronic back pain, as Dr. Apkarian revealed, causes more than just pain in the back or neck since it appears to cause cerebral degeneration/chemical alterations, but they admit “a single mechanism is as of yet not known.”
“Chronic pain patients suffer from more than just pain; depression and anxiety, sleep disturbances, and decision-making abnormalities (Apkarian et al., 2004) also significantly diminish their quality of life. Recent studies have demonstrated that chronic pain harms cortical areas unrelated to pain (Apkarian et al., 2004; Acerra and Moseley, 2005), but whether these structural impairments and behavioral deficits are connected by a single mechanism is as of yet unknown.”[60]
How ironic would it be if spinal dysfunction begun during youthful sport injuries, falls in the home, or car accidents were the instigators of this malady—problems that chiropractic spinal care could alleviate. Imagine the amount of pain and disease that could have been alleviated by chiropractors if the medical boycott had never occurred and everyone had access to our brand of care.
Chiropractic Care Recommended for Fibromyalgia
Not only can chronic back pain shrink the brain, other scientists now believe degenerative disorders of the central nerve system may be responsible for fibromyalgia, chronic fatigue, post-traumatic stress disorder, irritable bowel syndrome, and depression, as well as the similarity of many CNS abnormalities.
More researchers found similar degeneration of the brains in women with fibromyalgia, which has traditionally been classified as either a musculoskeletal disease or a psychological disorder.
In a study published in The Journal of Neuroscience in 2007 by Anil Kuchinad et al., MRI scans of the brains of 10 female fibromyalgia patients and 10 healthy controls found that fibromyalgia patients had significantly less total gray matter volume and showed a 3.3 times greater age-associated decrease in gray matter than healthy controls.[61]
The longer the individuals had had fibromyalgia, the greater the gray matter loss, with each year of fibromyalgia being equivalent to 9.5 times the loss in normal aging. In addition, fibromyalgia patients demonstrated significantly less gray matter density than healthy controls in several brain regions…The neuro-anatomical changes that we see in fibromyalgia patients contribute additional evidence of CNS involvement in fibromyalgia.
In particular, fibromyalgia appears to be associated with an acceleration of age-related changes in the very substance of the brain. Moreover, the regions in which we demonstrate objective changes may be functionally linked to core features of the disorder including affective disturbances and chronic widespread pain.
Fibromyalgia’s defining features (chronic widespread pain and tenderness to palpation) may be explained by the mechanism known as “sympathetically maintained pain.” After a triggering event (physical/emotional trauma, infections) relentless sympathetic hyperactivity may develop in susceptible individuals. This hyperactivity induces excessive norepinephrine (also known as noradrenalin) secretion that could in turn sensitize central and peripheral pain receptors and thus induce widespread pain and widespread tenderness. [62]
Patients with fibromyalgia have relentless hyperactivity of the sympathetic nerve system, aka, hyper-sympathetictonia. The results of these studies suggest that a fundamental alteration of fibromyalgia is a disordered function of the autonomic nerve system. Patients with fibromyalgia have a relentless sympathetic hyperactivity throughout 24 hours. This may explain the sleeping problems that the patients have because they never attain the parasympathetic state of “rest and digest” because the sympathetic nerve system keeps firing.
At the same time, such individuals have sympathetic hypo-reactivity to stress, which could explain the profound fatigue, morning stiffness and other complaints associated to low blood pressure. This autonomic nerve system dysfunction could induce other symptoms of fibromyalgia such as irritable bowel, urinary discomfort, limb numbness, anxiety and dryness of the eyes and mouth.[63]
Musculoskeletal Disorders Misdiagnosed as FMS
Drs. Schneider, Brady and Perle wrote a compelling paper suggesting that patients with fibromyalgia (FMS) may often be misdiagnosed due to the ambiguity of the widespread pain in multiple body regions, the character and distribution of this widespread pain are typically poorly described by the patient as vague and diffuse, and most MDs simply fail to diagnose properly.[64]
To the average MD, the authors suggests this presents a “diagnostic conundrum because of generally poor knowledge about musculoskeletal disorders within primary care medicine,” plus the fact that standard internal medicine textbooks present limited potential etiologies and diagnoses for these kinds of pains.[65]
Schneider et al. show there are well-documented pain generators in the musculoskeletal tissues that are not typically recognized by MDs whose training is more focused on visceral referred pain patterns rather than somato or spine referred pain. Bogduk et al. have shown it is common for patients to present with pains that clearly emanate from spinal facet and sacroiliac joints.[66],[67]
Unfortunately, the diagnosis of facet and sacroiliac joint pain is not a simple matter for those clinicians who rely solely upon imaging studies because there is not necessarily any pathoanatomical changes in these joints associated with the referred pain patterns. As the NZ Report mentioned, just as you cannot see a headache or limp on x-ray, nor can you see joint dysfunction.
Actually, for decades the medical profession believed the sacroiliac joints couldn’t move, which proved to be wrong, and secondly, because there are no discs in these joints, many ignored the sacroiliac as a source of pain, which is another big mistake.
Consequently, these unusual patterns of back or neck pain coupled with negative diagnostic imaging studies might lead the unwary medical clinician to declare FMS as the diagnosis when, in reality, the pain is emanating from the facet or sacroiliac joints, conditions helped greatly by spinal manipulation.
Schneider and his colleagues conclude:
Lastly, many common musculoskeletal conditions can mimic FMS. It is imperative that the clinician understand the many musculoskeletal sources of unusual referred pain patterns that could be misdiagnosed as FMS. A careful physical examination by a clinician with experience in musculoskeletal differential diagnosis would help to sort out more of these cases, which could potentially reduce the error rate of FMS misdiagnosis. [68]
Just as Nansel recommended, Schneider urges “collaborative patient management between clinicians, chiropractors, osteopaths, and physical therapists would seem to be the best way to ensure that patients with these musculoskeletal causes of widespread pain would receive the appropriate diagnosis and therapy, without resorting to a default diagnosis of FMS in all cases of widespread pain.”
To the surprise of many, this viewpoint has been acknowledged by some important guidelines that rely on evidence-based criteria and now recommend chiropractic care for the treatment of fibromyalgia.[69]
The American College of Occupational and Environmental Medicine (ACOEM) recommends chiropractic care in its Occupational Medicine Practice Guidelines treatments for several chronic pain conditions including complex regional pain syndrome (CRPS), neuropathic pain, trigger points/myofascial pain, chronic persistent pain, fibromyalgia and chronic low back pain. The recommendations are based on more than 1,500 references, including 546 randomized, controlled trials.[70]
ACOEM’s latest chronic pain guidelines represent a step in the right direction in terms of recognizing the value of chiropractic care. The guidelines also recommend manipulation for chronic, persistent low back or neck pain and cervicogenic headache.
The American Academy of Family Physicians published “Treating Fibromyalgia” and admitted this elusive disorder is not psychosomatic, but is directly associated with “musculoskeletal pain unrelated to a clearly defined anatomic lesion” and that chiropractic treatment has proven effective. [71]
The AAFP Guideline now recommends chiropractic treatment for fibromyalgia, citing a pilot study by KL Blunt et al in which following four weeks of treatment, 21 patients with fibromyalgia improved compared with control subjects receiving medication only.[72]
Again, the mechanism of this improvement — the how and the why — may lie deep within the cranium initiated by neurotransmitters and spinal stress years before; it may be an imbalance or gibberish within the autonomic nerve system or a spinovisceral reflex, but the evidence reveals that reducing back pain may decrease the degeneration at the core of this malady.
The research that now reveals that chronic back pain may lead to degeneration of the brain is a good example of finally seeing the forest through the trees. What may have begun as a common childhood fall off a bicycle that injuries the spine may later lead to a life of chronic back pain, which in turn may develop into fibromyalgia, chronic fatigue, post-traumatic stress disorder, irritable bowel syndrome, and depression as the researchers now suggest.
As you can see, today’s chiropractic is not the old “pinched nerve” theory although that was a reasonable starting point one hundred years ago. Neurophysiologists now suggest the effects of a bad back may lead to a myriad of problems such as somatovisceral reflexes, dysautonomia, and cerebral degeneration via altered neurotransmitters.
Indeed, today’s chiropractic is not what our grandfather knew. Now you can understand the madness behind our methods rather than just believing in the results. For those skeptics, this research validates the importance of a healthy spine and the role chiropractic care may have upon pain syndromes and organic disorders.
Chiropractic Cures All?
I have saved the most controversial aspect of chiropractic for the last to give you some good food for thought about health that transcends the physical into the meta-physical, an issue the medical profession inherently dislikes, but the ol’ time chiropractors embrace as its unique philosophy.
Since these early chiropractors at the time couldn’t explain the art and science in convincing scientific terms inasmuch as neurophysiology was virtually unknown at the time, just as the medical science was evolving from leeches, demons and bloodletting, so they turned to metaphysical explanations of chiropractic that was difficult for medical practitioners to swallow.
Joseph C. Keating, Jr., PhD, noted chiropractic historian, discusses vitalism’s past and present roles in chiropractic and calls vitalism “a form of bio-theology” that he views as incompatible with scientific thinking:
“Chiropractors are not unique in recognizing a tendency and capacity for self-repair and auto-regulation of human physiology. But we surely stick out like a sore thumb among professions which claim to be scientifically based by our unrelenting commitment to vitalism. So long as we propound the ‘One cause, one cure’ rhetoric of Innate, we should expect to be met by ridicule from the wider health science community. Chiropractors can’t have it both ways. Our theories cannot be both dogmatically held vitalistic constructs and be scientific at the same time. The purposiveness, consciousness and rigidity of the Palmers’ Innate should be rejected.” [73]
This “one cause-one cure-one correction” attitude by both DD and BJ Palmer created the “cure-all” belief that so irritated the medical profession, and understandably so. This is the source of the strongest criticism of chiropractors: “They go too far when they claim chiropractic care can cure everything.” I’ve never heard or read any reliable chiropractor proclaim this today although, as you have learned, the impact of a vertebral subluxation or spinal lesion upon your homeostasis and the brain itself may explain why this is possible. Indeed, this is a holdover from 100 years ago that still haunts the profession not because it is untrue, but that it is poorly understood.
At this point, most chiropractors would just be happy if the medical society would admit we’re good for most musculoskeletal disorders, an issue they still resist despite the overwhelming evidence by their own researchers.
While the Palmers may have embellished the belief that since the nerve system influences all tissues in the body, any spinal injury could potentially cause dysfunction elsewhere. Of course, most DCs flinch at this idea today for fear of arousing the medical wrath and the skepticism of the public since few people understand neurophysiology and events like somatovisceral reflex disorders.
The Founder of Chiropractic, DD Palmer, attempted to explain the mechanism of chiropractic when he published in 1910 his 984-page book, “The Science, Art and Philosophy of Chiropractic.” [74] D.D. Palmer’s effort to find the cause for disease led him to write:
One question was always uppermost in my mind in my search for the cause of disease. I desired to know why one person was ailing and his associate, eating at the same table, working in the same shop, at the same bench, was not … This question had worried thousands for centuries and was answered in September, 1895.
Harvey Lillard, a janitor, in the Ryan Block, where I had my office, had been so deaf for 17 years that he could not hear the racket of a wagon on the street or the ticking of a watch. I made inquiry as to the cause of his deafness and was informed that when he was exerting himself in a cramped, stooping position, he felt something give way in his back and immediately became deaf. I reasoned that if that vertebra was replaced, the man’s hearing should be restored. With this object in view, a half-hour’s talk persuaded Mr. Lillard to allow me to replace it. I racked it into position by using the spinous process as a lever and soon the man could hear as before.
… Shortly after this relief from deafness, I had a case of heart trouble which was not improving. I examined the spine and found a displaced vertebra pressing against the nerves which innervate the heart. I adjusted the vertebra and gave immediate relief … Then I began to reason if two diseases, so dissimilar as deafness and heart trouble, came from the impingement, a pressure on nerves, were not other diseases due to a similar cause? Thus the science (knowledge) of Chiropractic were formed at that time. I then began a systematic investigation for the cause of all diseases and have been amply rewarded.[75]
Obviously his neurogenic theory conflicted with the allopaths who believed in the germ theory as the primary cause of disease. Medical science was still quite primitive and certainly unaware of the role of spinal stress upon the nerve system to cause health problems, so the battle line was drawn. Apparently only one cause of disease could exist and the germ theory dominated.
Virgil Strang explained the early chiropractic philosophy:
The problem with trying to mesh chiropractic philosophy with science was that science at that time was still mainly mechanistic in its conceptualizations. Therefore, scientists were still quick to reject any form of vitalism.
From the very beginning days of chiropractic, there was a realization within the profession that the mechanistic philosophy of the allopaths was obviously missing something; their philosophy simply was unable to account for the fact that all of life seems to possess an organizing, purposeful force. In an attempt to remedy this situation, DD Palmer used the exquisite phrases “Universal Intelligence” and “Innate Intelligence” to speak of the organizing force that pervades everything from the vast galaxies to the simple squamous cells of the epithelium.
One must remember that DD Palmer was writing at a time when important mechanisms of neurology, homeostasis and genetics were still to be discovered. It was the age before scientific thinking was turned on its ear by the development of the concepts of energy and field in electro-magnetism, light, gravitation and the atom… there are today solid parallels in science which can allow us to assume with more confidence than ever that there is an overall organization in living matter which can be (and should be) accounted for by chiropractic philosophy…
The interesting think about scientific research is that as it has unfolded over the past 100 years, the findings have invariably supported the major premises of chiropractic. Scientific research has done one thing in the 20th century for chiropractic philosophy: it has enabled us to now present a stronger case for the presence of intelligence (an organizing force) in both the universe and the human organism.[76]
Perhaps now research by A. Vania Apkarian, P. Schweinhardt, Acerra, Moseley, Sato, Budgell, and Anil Kuchinad is finally catching up to explaining the why and how spinal manipulation may affect nerve system function and overall homeostasis.
Actually, compared to the medical germ theory, this chiropractic theory was far advanced as an explanation of chronic degenerative diseases. Perhaps some of the anger of the medical society stems from jealousy inasmuch as germs have little, if any, impact upon chronic degenerative diseases. Indeed, just as the disc theory is dying, so too the germ theory is on its last leg.
Instead of exploring this chiropractic theory, the political medicine headed by Morris Fishbein chose to ridicule anything chiropractic said to maintain its hold upon the healthcare professions. Plus, there was always from outlandish statements by some “wild-eyed” chiropractor to fuel their fire, and at the top of this list was the concept of vitalism.
To Believe or Not to Believe is the Question
Not only does the AMA oppose free enterprise in healthcare from its bully pulpit, many also have embraced a rather shocking attitude that shuns any mention of a God factor in healthcare. Without question, this combination of bullies and atheism is a big problem for any effort to reform healthcare.
In fact, the majority of MDs and elite scientists allegedly are atheists, which explains their unconscionable position that is devoid of justice, tolerance, or love. Instead, the AMA has been “relentless” and “objectively unreasonable” as the NZ Commission and the Wilk trial judge both found.
This is also the unnerving admission by Francis R. Collins, MD, author of The Language of God, The Language of Life, the past director of the Human Genome Project, presently the Director of the National Institutes of Health, and undoubtedly the most powerful MD in the nation today.
From his personal experience, Dr. Collins admits as many as sixty percent of doctors and scientists are atheists.[77] Dr. Collins spoke of his experience in medical school when the prevailing academic dogma to be strictly scientific ridiculed any supernatural belief in the God factor in the healing process. Indeed, if you were really smart, students were told, you cannot believe in God.
He addressed this conflict between vitalism and medical science when he said for many “faith can be seen as an enemy”:
Scientists believe in that they are very troubled by a suggestion that other kinds of approaches can be taken to derive truth about nature. And some I think have seen faith as therefore a threat to the scientific method and therefore it to be resisted.
I think for many scientists, particularly for those who have seen the shrill pronouncements from extreme views that threaten what they’re doing scientifically and feel therefore they can’t really include those thoughts into their own worldview, faith can be seen as an enemy.
And similarly, on the other side, some of my scientific colleagues who are of an atheist persuasion are sometimes using science as a club over the head of believers basically suggesting that anything that can’t be reduced to a scientific question isn’t important and just represents superstition that should be gotten rid of.
Part of the problem is, I think, the extremists have occupied the stage. Those voices are the ones we hear. I think most people are actually kind of comfortable with the idea that science is a reliable way to learn about nature, but it’s not the whole story and there’s a place also for religion, for faith, for theology, for philosophy. But that harmony perspective does not get as much attention, nobody’s as interested in harmony as they are in conflict, I’m afraid. [78]
It is troubling to think the majority of medical doctors are atheists who scoff at the God factor in health. How many God-fearing patients would respect or trust their MDs if they knew they were atheists? Ironically, their denial of an innate vital force appears to be their own folly as healers.
Despite their own Hippocratic roots, medical scientists and practitioners clothe themselves in scientism with a total disdain for vitalism. To this day, this conflict prevails. Stephen Hawking, the Lucasian Professor of Mathematics at Cambridge University, has said “Scientists can’t prove that God doesn’t exist, but science makes God unnecessary.”[79]
This is the mindset of modern American medical profession as well. Apparently these minor deities (MDs) have no room on their medical pedestals for the major deity.
NM Hadler, MD, author of Stabbed in the Back, (a good description of medicine’s attack on chiropractic) spoke of his medical chauvinism with pride:
I admit to chauvinism; I value my profession above all others to the extent that it tests the limits of certainly regarding the validity of its therapeutic offerings. I write extensively on how the institution of contemporary medicine has lost its way, but I also write extensively on how its practitioners hear a higher calling.[80]
If his admission to “chauvinism” and a “higher calling” is not evidence of a supremacist attitude, what is?
American medicine has become so cynical that a simple belief in the God factor is now a professional sin that should be shunned. In effect, these scientists and MDs have taken the “bio” out of biology—in other words, the life that gives vitality, vim, and vigor to a living body—the God factor.
I am not suggesting faith healing or superstitious beliefs alone are all that is required in the healing process, nor am I saying all disease is psychosomatic. Certainly medical interventions have been a blessing to many patients especially in emergency situations. As well, chirovangelism alone is just as inadequate as a dose of drugs.
But these atheists refuse to admit the human body is a vital entity consisting of physical and meta-physical components. We are not inanimate machines devoid of any God factor. Even the recent discovery of the Higgs boson God particle is evidence of a supernatural factor in the universe that glues everything together.
Surprisingly, the original Medical Mussolini himself, Morris Fishbein, reportedly spoke of the God factor in the healing process.
“Never must the physician say, ‘the disease is incurable.’ By that admission he denies God, our Creator; he doubts Nature with her profuseness of hidden powers and mysteries.”[81]
This atheistic attitude in the medical profession is a relatively new position considering the vitality within the body to heal was coined by the early medical profession as the Vis Medicatrix Naturae – the healing power of nature.[82]
From this follows the belief that “nature is the best physician” or “nature is the healer of disease.” Hippocrates considered a doctor’s chief aim was to help this natural tendency of the body by observing its action, removing obstacles to its action, and thus allow an organism to recover its own health.[83]
However, the medical atheists now decry any mention of a God-factor, choosing instead to believe they are replacing the superstitions of the past with scientific beliefs. They want to promote enlightenment over dogma, but in this quest, they ignore the primordial aspect of health and life itself—the God factor—that is the difference between life and death, health and disease.
In an attempt to appear scientific, modern medical practitioners cloak themselves in scientism with a total disdain for vitalism. Ironically, their denial of an innate vital healing force appears to be their own folly.
Indeed, modern medicine has lost its soul by embracing an atheistic attitude.
Élan Vital, Vitalism and Chiropractic
Part of the problem with MDs is their limited perspective of health. Being the supposed “scientific” profession that uses only mechanistic, physical science to explain itself, health has become a function mainly of MRI scans, blood analysis and other quantifiable tests. Indeed, most folks are fully aware of their blood counts such as cholesterol levels, triglycerides, and sugar levels, but they often miss seeing the forest through these medical trees.
What’s been lost today in medical science are the intangible elements that focuses on the patient’s overall health. Terms such as “vim”, “vigor” and “vitality” are lost in today’s scientific arena since they cannot be measured, but they remain descriptions of good health. Too many patients may have perfect blood profiles, but they lack the vitality associated with vibrant health. If it is not “bad blood”, what else could it be — perhaps “bad nerves” or “bad diets” or “bad attitudes” about health in general?
Chiropractic’s tribulation with medical acceptance were compounded by the Palmers’ belief of vitalism in the healing process. Vitalism, as defined by the Merriam-Webster dictionary, is “a doctrine that the functions of a living organism are due to a vital principle distinct from physio-chemical forces.”
Obviously the medical profession, built on bio-chemical concepts of pharmacology and the mechanistic belief in surgery, has little room in its ideology for anything immaterial in its quest to appear scientific although medical guru David Eddy, MD, PhD, admits only 15% of medical procedures are based on scientific evidence. [84]
The original Palmer tenets suggested that not only do “mental impulses” flow along the nerves, but a “life force” does too. Any interference to this flow of life-sustaining energy will cause dysfunction or what Palmer describes as a state of “dis-ease.” While the premise sounds plausible to some, it has never been proven in the science laboratory, although anecdotal evidence in DC offices has existed for 110 years.
Apparently the public has an easier time accepting vitalism in chiropractic care. For example, in 1984, the Chiropractic Association of Oklahoma surveyed 400 households seeking their “attitudes toward chiropractic health care in Oklahoma.”[85] The results were interesting to say the least and provoking in what they revealed. Most interesting was that the more controversial aspects of chiropractic treatment and philosophy — the affect upon organic function and the concept of vitalism — was also very well received by the public.
“Some of the axioms around which chiropractic is structured are firmly believed in, and these are the ones which should be promoted more stringently since they will reach a higher degree of sympathetic belief. A particularly high number (over eight out of ten) agree that:
1. Once nerves are involved, almost anything can go wrong.
2. Bones in the spine can pinch or get out of alignment and affect functions.
“Additionally, a very high number (71% to 75%) also agree that:
1. The spine can easily get out of alignment and affect functions
2. Nerves more than anything regulate function.
3. There is an unseen life force that cannot function unless all is in harmony.” (emphasis added)
This poll shows the paradox in healthcare: while health professions pride themselves on being scientific in this era of evidence-based medicine, the public also recognizes the inherent self-regulation of the body known as vis medicatrix naturae and the healing power of Nature or God. But few health professionals want to acknowledge it and certainly when chiropractors speak of this innate healing force, red flags go up by apoplectic MDs who scream “quackery.”
According to David Eisenberg, MD and Ted Kaptchuk, OMD, vitalism is a trans-professional concept.
Alternative medicine offers a person threatened by illness or disease a connection with fundamentally benign, lawful, coherent, potent, and even meaningful powers. When illness isolates, alternative health care allows a rescuing connection to life-supporting cosmic forces. This vital energy takes myriad forms: homeopathy speaks of a “spiritual vital essence”, chiropractic refers to the “innate”, and acupuncture is said to involve the flow of “qi”. Ayurvedic medicine is based on the power called “prana”, and new age healing practices work with “psychic” or “astral” energies. The alternative alliance routinely claims that its methods rely on enhancing “life forces” as opposed to “destroying” them with artificial drugs and surgery.[86]
Although both the public and the Palmers recognize this innate healing force, it is taboo as an explanation according to historian Joseph Keating: “in this context, Innate becomes a label for the unknown and so long as the label is not mistaken for an explanation (i.e., for the ‘known’) no supernatural intrusion upon science occurs.”[87]
Even though today most chiropractors do not make such “scientifically-incorrect” claims, those who believe in the power of the body to heal itself via the proper functioning of the nerve system have created an image that is both hard to support and hard to deny.
Ironically, on Sundays even the MDs pray for health and peace, but on Mondays they wage a holy war on vitalism and denounce the chiropractors as quacks for suggesting there is an élan vital in the healing process.
DD Palmer wrote that “Life is but the expression of spirit thru matter.”[88]
Why the medical profession thinks it is heretical to science to speak of the spirit in the living matter has always been a shortcoming and not a tribute to its reductionist, mechanistic beliefs.
I daresay every chiropractor or MD can attest to some rather remarkable healing that transcends the explainable science of our present understanding. The problem remains it is hard to base an entire profession on the unexplainable, which has led to strong criticism by medical professionals who are opposed to anything that appears faith-based healthcare.
But to some ol’ time chiropractors, this is their raison de’tat—their prime philosophy of practice—to liberate the nerve energy that carries the life force to every cell in the human body. This is their chiropractic philosophy also known as vitalism that is condemned by scientific medicine and make evidence-based chiropractors wince.
The developer of chiropractic, BJ Palmer, and many of his disciples have even made a pseudo-religion—chirovangelism—of this vitalism and this has been a source of controversy for over 110 years now. It is one thing to blend the spirit with the matter as DD Palmer did, but it is totally another issue to ignore the science of the matter as the chirovangelists have done.
Most of the bad press concerning cultism and quackery in chiropractic stems from these chiropractors who subscribe to the demagoguery espoused by BJ Palmer and Sid Williams. Recall that BJ was allegedly denounced in the Illinois Medical Journal as “the most dangerous man in Iowa outside a prison cell,” [89] not for what he did clinically but for what he said.
After DD Palmer’s death in 1913, BJ became Developer of chiropractic during the early 20th century when chiropractors were being prosecuted for practicing medicine without a license. The Palmers created their metaphysical explanation because DD, BJ and their followers couldn’t explain the mechanisms of their art in scientific terms; plus this philosophy became a legal ploy to avoid being accused of practicing medicine or osteopathy.
The most basic example is the “spirit” or life energy that distinguishes living from non-living matter. Indeed, what is missing in a dead body? Every physical attribute is still there—the brain and nerves, the heart and blood, the bones, organs and muscles. Nothing is missing in a dead body except for the vital force that animates the living.
In 1951 BJ Palmer wrote a letter to Dr. Marchus Bach of the School of Religion, State University of Iowa, regarding the difference between “Cult vs. Science.”
“The difference between a ‘cult’ and a ‘science’ is that a ‘cult’ is mental with no matter; a ‘science’ is matter with no mental. Chiropractic unites the mental AND matter and makes them work together. Chiropractic therefore is, strictly, neither a ‘cult’ NOR a ‘science.’”[90]
At the 1959 Homecoming at Palmer College of Chiropractic, BJ Palmer gave this speech exemplifying the chirovangelism of ol’ time chiropractic:
“In studying Innate, we have accomplished what all religions have always wanted to do, viz., make ‘The Kingdom of God Is Within You’ a tangible working integral part of living man. We have accomplished what medical therapies have always failed to do but wanted to do, viz., found a specific cause for all dis-ease (as there is but one) and a specific for the correction of that cause, thus making a living healthy sane God live healthily and sanely in man.”
“‘Verily, I say unto you, all power cometh from within,’ is no longer a mysticism of the East, but a practical, working, human principal of the West. Chiropractors who apply the science are proving the wisdom of Him who said, ‘there is nothing from without a man that entering into him can defile him,’ germ theorists and dietitians, notwithstanding.”
“Innate is God in human beings; is good in human beings, is life in human beings, is health in human beings, is sane in human beings. Let Innate flow in and through us and we can accomplish the great wonders.”
“Within us, it is said “The Kingdom of God is within you.” It is! Innate Intelligence is the Great I am that I am. Innate Intelligence is the internal source of all and everything.”
“Within all natural animals, including man and woman, courses in active flow the wisdom of all time, the sage of the ages call it what you may—Universal Intelligence, God, Jehovah, etc.”
“May God flow from ABOVE-DOWN its bounteous strengths, courages, and understandings to carry on; and may your Innate receive and act on that free flow of wisdom from ABOVE-DOWN-INSIDE-OUT; for you HAVE in YOUR possession a sacred trust. Guard it well.”
“Theles (about 500 BC) saw fit to think he had divided man. The soul, spirit—what we Chiropractors call Innate Intelligence—was one half.
This half was given to religions, theosophies, etc. The corporeal, matter was the other half. This was given to physicians because they studied, taught, prescribed and practiced with and upon the physical.”
“Chiropractic is almost a LIVING GOD-like religion IN MAN which no man has any right to TRY TO CAST OUT OF MAN, OR TO SAY THAT GOD IN MAN MUST GO, merely because some are so blind they can’t see, so deaf they won’t hear, so insensible they can’t sense its greatness IN man as a living entity…Yet perhaps Chiropractic—its philosophy offers the best understanding of the relationship of God and man that can be found in any of our philosophies.”[91]
While BJ Palmer’s speech is appealing to those chiropractors who seek a spiritual link between God and chiropractic — chirovangelism — it is next to impossible to speak of this metaphysical power to evidence-based people who cherish the scientific principles—they want proof, measurements, and the ability to duplicate it in the laboratory. Case studies, anecdotal evidence, philosophy or bio-theosophy is not enough to convince these hard core scientists, even when the evidence is obvious. Indeed, ultimately they must ask: what is the primordial difference between life and death?
NM Hadler, MD, author of “The Last Well Person,”[92] scoffs at the vitalism found in some chiropractic enclaves.
“What is less defined, somewhat contentious within chiropractic, and very contentious for mainstream medicine is the purview of the chiropractic. Is it solely the regional musculoskeletal disorders? That is not the stance of many chiropractors or many schools of chiropractic. These advocates and practitioners are willing to ‘reduce subluxations’ for a range of ailments from headaches to asthma.”
“Subluxations are the chiropractic diagnosis that implies spinal malalignment. They are imaginary; no such specific skeletal changes correlate with symptoms…how anyone can imagine that such an event can salve asthma or diabetes or the like is a testimony to the tenacity of vitalistic theories.”
What Hadler suggests typifies another Fundamental Flaw of mechanistic medicine—the ingrained dislike of any vitalistic concept, whether it’s by ol’ time chiropractors or Traditional Chinese Medicine, Christian Scientists or anyone who speaks of the vital energy within the body—that immaterial intelligence that animates the physical—including religious leaders who speak of the mind, faith, and soul connection in healing. He also shows his ignorance of homeostasis, neurophysiology, and neuro-chemistry; as we’ve seen, these do play a role in the Type O ailments shown to be helped by manipulative therapy.
Apparently many MDs may believe in God to heal, but will criticize those who profess the same “hidden powers” are important in the healing process. It was the same contradictory attitude by Fishbein who prayed to a loving God as he crucified chiropractors.
This is the conflict between science-based vs. faith-based practitioners is not just a chiropractic dilemma. George Lundberg, MD, Medscape Editor in Chief, former editor-in-chief of JAMA from 1982 to 1999, spoke of this faith-based phenomenon in medicine in his webcast editorial.[93]
“Recognizing that not all interventions have been properly studied but that physicians must make clinical decisions anyway, David Sackett is credited with having defined EBM as the ‘integration of best research evidence with clinical expertise and patient values.’
“I consider the near opposite of pure EBM to be pure FBM — faith-based medicine. St. Paul defined faith as ‘the substance of things hoped for, the evidence of things unseen.’ This was OK for medicine in the first century AD, but in 2004, when there is evidence, I choose it as the basis for my care.”
Apparently many medical experts remain critical of “things hoped for but unseen” in treatments, but the lack of evidence for many medical treatments consisting of drugs, shots, and surgery has not diminished their use, even when the call for reform grows louder.
Indeed, just how long has the war on cancer lingered on although medicine still hopes for a solution that apparently does not rest with drugs or surgery? Chiropractic ethicist Dr. Louis Sportelli mentioned this dilemma of searching only for allopathic treatments in the war on disease:
“We’ve been overlooked for a long time. People think we just take care of backaches and headaches, and we do that, but there are much broader dimensions … It’s time to cast aside some pre-conceived prejudices and explore new solutions. There’s so little money for drugless research generally. All the emphasis in our society is on chemical cures.”[94]
Certainly there is more to healthcare than only the physical or chemical components, which explains why many Americans are using holistic complementary and alternative methods today. Many evidence-based DCs are also torn with this dilemma, myself included, because the evidence points in both directions.
Recall DD Palmer’s conundrum when he initially helped a deaf janitor and a man with heart disease. Rather than being limited in his critical thinking to the prevailing medical germ theory, he was among the first to think out of the medical black bag for an explanation and he looked at the Master System for the answer.
Indeed, medical or any healthcare science certainly is not exact; in other words, 1 + 1 does not always equal 2. To deny the role of emotions, stress, positive thinking or faith in the healing process is naïve and denies the obvious—in fact, it may be the unknown x-factor in the healing process.
Yet every doctor is aware of the value of a positive attitude in healing whether it is called faith or the placebo effect, a belief in a healing power will always be a part of this equation. Whether or not chiropractic adjustments of the spine have any affect upon this healing power in a spiritual sense will always be a point of contention since God only knows, but science now has shown that manipulation of spinal joints does affect the neurophysiology of your body, a concept still needing to be explored and explained to the public.
It’s time to stop the suffering; it’s time to start cooperating. It’s time for a new paradigm in healthcare that includes all factors of healing.
[1] Strang, VV. Essential principles of chiropractic, Palmer College of Chiropractic, Davenport, 1984. p. 126.
[2] Palmer, ibid. p. 233.
[3] Relief for aching backs, Consumer Reports, May 2009.
[4] Romano, Lois. Riding Accident Paralyzes Actor Christopher Reeve. Washington Post, June 1, 1995, pg. A01. Accessed November 19, 2006.
[5] Christopher Reeve Homepage. Christopher Reeve Testimony: April 26, 2000. Accessed November 30, 2006.
[6] Meeker, WC and Haldeman, S, Chiropractic: a profession at the crossroads of mainstream and alternative medicine, American College of Physicians-American Society of Internal Medicine, Ann Intern Med. 2002; 136:216-227, p. 222.
[7] Hondras MA, Long CR, Brennan PC. Spinal manipulative therapy versus a low force mimic maneuver for women with primary dysmenorrhea: a randomized,observer-blinded, clinical trial. Pain. 1999;81:105-14. [PMID: 10353498]
[8] Kokjohn K, Schmid DM, Triano JJ, Brennan PC. The effect of spinal manipulation on pain and prostaglandin levels in women with primary dysmenorrhea. J Manipulative Physiol Ther. 1992;15:279-85. [PMID: 1535359]
[9] Morgan JP, Dickey JL, Hunt HH, Hudgins PM. A controlled trial of spinal manipulation in the management of hypertension. J Am Osteopath Assoc. 1985;85:308-13. [PMID: 3900016]
[10] Yates RG, Lamping DL, Abram NL, Wright C. Effects of chiropractic treatment on blood pressure and anxiety: a randomized, controlled trial. J Manipulative Physiol Ther. 1988;11:484-8. [PMID: 3075649]
[11] Balon J, Aker PD, Crowther ER, Danielson C, Cox PG, O’Shaughnessy D, et al. A comparison of active and simulated chiropractic manipulation as adjunctive treatment for childhood asthma. N Engl J Med. 1998;339:1013-20. [PMID: 9761802]
[12] Nielsen NH, Bronfort G, Bendix T, Madsen F, Weeke B. Chronic asthma and chiropractic spinal manipulation: a randomized clinical trial. Clin Exp Allergy. 1995;25:80-8. [PMID: 7728627]
[13] Reed WR, Beavers S, Reddy SK, Kern G. Chiropractic management of primary nocturnal enuresis. J Manipulative Physiol Ther. 1994;17:596-600. [PMID: 7884329]
[14] Wiberg JM, Nordsteen J, Nilsson N. The short-term effect of spinal manipulation in the treatment of infantile colic: a randomized controlled clinical trial with a blinded observer. J Manipulative Physiol Ther. 1999;22:517-22. [PMID:10543581]
[15] Walsh MJ, Polus BI. A randomized, placebo-controlled clinical trial on the efficacy of chiropractic therapy on premenstrual syndrome. J Manipulative Physiol Ther. 1999;22:582-5. [PMID: 10626701]
[16] Hazzard C: Principles of Osteopathy, 3rd edition. Kirksville, MO, Charles Hazzard, 1899.
[17] Keating, JC, Toward a Philosophy of the Science of Chiropractic, 1992, pp. 15.
[18] Keating, JC, D.D. Palmer’s Forgotten Theories of Chiropractic, A Presentation to the Canadian Memorial Chiropractic College, February 18, 1995.
[19] Palmer, DD, The Chiropractor’s Adjuster, Portland Printing House Company, 1910. p.7
[20] Keating, Joseph C. Jr., PhD, D.D. Palmer’s Forgotten Theories of Chiropractic, A Presentation to the Canadian Memorial Chiropractic College, February 18, 1995.
[21] Sesso, Howard D., ScD, MPH; Julie E. Buring, ScD; Nader Rifai, PhD; Gavin J. Blake, MD, MPH; J. Michael Gaziano, MD, MPH; Paul M. Ridker, MD, MPH, C-Reactive Protein and the Risk of Developing Hypertension, JAMA. 2003;290:2945-2951.
[22] Korr, IM, Spinal cord as organizer of disease process. Academy of Applied Osteopathy Yearbook, 1976.
[23] Irvin Korr Ph.D. (1909–2004) obituary, Journal of Bodywork and Movement Therapies (2004) 8, 155–157
[24] Strang, VV. Essential principles of chiropractic, Palmer College of Chiropractic, Davenport, 1984.
[25] Strang, ibid. p. 48.
[26] Williams and Warwick, eds., Gray’s Anatomy, 36th ed. (London: Saunders, 1980, p.72).
[27] Strang, ibid. p. 50.
[28] Strang, ibid. p. 57.
[29] Palmer, ibid. p. 57.
[30] Korr IM, Appeltauer GSL. Trophic functions of nerves. In: Beal MC, ed. 1994 Yearbook: Louisa Burns Memorial. Indianapolis, Ind: American Academy of Osteopathy; 1994:52 -60.
[31] Still AT. Autobiography of Andrew T. Still. Kirksville, Mo: AT Still; 1897.
[32] Korr I M, ‘The Collected Papers of Ivan M. Korr’ (1979), American Academy of Osteopathy, Newark Ohio.
[33] Vernon H T, Dhami M S et al (1986) ‘Spinal Manipulation and Beta-Endorphin: A Controlled Study on the Effect of a Spinal Manipulation on Plasma Beta-Endorphin Levels in Normal Males’, J. Manipulative Physio Ther 9(2): 115-123.
[34] Vernon, ibid.
[35] Jarmel, Mark E., DC, a paper, “Possible Role of Spinal Joint Dysfunction in the Genesis of Sudden Cardiac Death,” Journal of Manipulative and Physiological Therapeutics, vol. 12-6, Dec. 1989.
[36] Jarmel M, DC, Zatkin J, PhD, et al., “Improvement of Cardiac Autonomic Regulation Following Spinal Manipulative Therapy,” Cleveland College of Chiropractic, LA, a paper presented at the Conference Proceedings of the Chiropractic Centennial Foundation, July 6-8, 1995.
[37] autonomic nerve system at Dorland’s Medical Dictionary.
[38] eMedicine/Stedman Medical Dictionary Lookup!”. Retrieved on 2008-11-30.
[39] Barbara Simpson, Human Anatomy And Physiology Biol, Origins Of Chronic Illness Part I, Pierce College, Wa
[40] Barbara Simpson, ibid.
[41] Bakris G. et al. Atlas vertebrae realignment and achievement of arterial pressure goal in hypertensive patients: a pilot study, J Hum Hypertens.2007 May;21(5):347-52. Department of Preventive Medicine, Rush University Hypertension Center, Chicago, IL, USA.
[42] Fogoros, Richard N., MD, Dysautonomia: A family of misunderstood disorders, About.com
[43] Fogoros, ibid.
[44] Millea, Paul J., M.D., M.S., Richard L. Holloway, Ph.D Treating Fibromyalgia, AAFP, http://www.aafp.org/afp/20001001/1575.html
[45] Budgell BS: Spinal manipulative therapy and visceral disorders. Chiropractic Journal of Australia, 1999, 29: 123-128.
[46] Nansel, D and Szlazak M, Somatic dysfunction and the phenomenon of visceral disease simulation: a probably explanation for the apparent effectiveness of somatic therapy in patients presumed to be suffering from true visceral disease, JMPT 1995 (July); 18(6): 379-397.
[47] Sato A, Sato Y, Schmidt RF: The Impact of Somatosensory Input on Autonomic Functions. Reviews of Physiology, Biochemistry and Pharmacology Vol 130, Springer-Verlag, Berlin, 1997.
[48] Pollard, Henry, Grad DC, MSportSc, PhD, Reflections on the “type O” disorder, JMPT, Volume 28, Issue 7, Pages 547.e1-547.e9 (September 2005).
[49] Pollard, ibid.
[50] Sato A Neural mechanisms of autonomic responses elicited by somatic sensory stimulation. Neurosci Behav Physiol; 27:610-21.
[51] Sato A, Sato Y, Schmidt RF. Changes in blood pressure and heart rate induced by movements of normal and inflamed knee joints. Neurosci Lett 1984;52:55-60.
[52] Budgell, Brian S. , DC Reflex effects of subluxation: the autonomic nerve system, J Maninulafive Physiol Ther 2000;23:104–6.
[53] Sato A, Swenson RS. Sympathetic nerve system response to mechanical stress of the spinal column in rats. J Manipulative Physiol Ther 1984;7:141-7.
[54] Bolton PS, Kerman IA, Woodring SF, Yates BJ. Influences of neck afferents on sympathetic and respiratory nerve activity. Brain Res Bulletin 1998;47:413-19.
[55] Fujimoto T, Budgell B, Uchida S, Suzuki A, Meguro K. Arterial tonometry in the measurement of the effects of innocuous mechanical stimulation of the neck on heart rate and blood pressure. J Autonom Nerv Syst 1999;75:109-115.
[56] Nansel, D and Szlazak M, Somatic dysfunction and the phenomenon of visceral disease simulation: a probably explanation for the apparent effectiveness of somatic therapy in patients presumed to be suffering from true visceral disease, JMPT 1995 (July); 18(6): 379-397.
[57] Seaman DR, Winterstein JF.Dysafferentation: a novel term to describe the neuropathophysiological effects of joint complex dysfunction. A look at likely mechanisms of symptom generation. J Manipulative Physiol Ther. 1998 May;21(4):267-80.
[58] A. Vania Apkarian et al. Chronic Back Pain Is Associated with Decreased Prefrontal and Thalamic Gray Matter Density
The Journal of Neuroscience, November 17, 2004, 24(46):10410-10415.
[59] Brendan Cosgrove, Northwestern University Newsfeed, Dr. Vania Apkarian on “Chronic Back Pain and the Brain,” November 29, 2004
[60] Baliki, Marwan N., et al. Beyond Feeling: Chronic Pain Hurts the Brain, Disrupting the Default-Mode Network Dynamics The Journal of Neuroscience, February 6, 2008, 28(6):1398-1403.
[61] Kuchinad, Anil et al. Accelerated Brain Gray Matter Loss in Fibromyalgia Patients: Premature Aging of the Brain? The Journal of Neuroscience, April 11, 2007, 27(15):4004-4007
[62] Martinez-Lavin M, Hermosillo AG, Mendoza C, et al. Orthostatic sympathetic derangement in individuals with fibromyalgia. J Rheumatol 1997;24:714.
[63] Martinez-Lavin, et al. ibid.
[64] Schneider, Michael J., DC, PhD, David M. Brady, ND, DC, and Stephen M. Perle, DC, MS, Commentary: Differential Diagnosis Of Fibromyalgia Syndrome: Proposal Of A Model And Algorithm For Patients Presenting With The
Primary Symptom Of Chronic Widespread Pain, J Manipulative Physiol Ther 2006;29:493- 501.
[65] Matzkin E, Smith ME, Freccero CD, Richardson AB. Adequacy of education in musculoskeletal medicine. J Bone Joint Surg Am 2005;87:310-4.
[66] Barnsley L, Lord S, Bogduk N. Comparative local anesthetic blocks in the diagnosis of cervical zygapophysial joint pain. Pain 1993;55:99-106.
[67]Dreyfuss P, Michaelsen M, Pauza KJ, McLarty J, Bogduk N. The value of medical history and physical examination in diagnosing sacroiliac joint pain. Spine 1996;21:2594-602.
[68] Schneider, Michael J., DC, PhD, David M. Brady, ND, DC, and Stephen M. Perle, DC, MS, Commentary: Differential Diagnosis Of Fibromyalgia Syndrome: Proposal Of A Model And Algorithm For Patients Presenting With The
Primary Symptom Of Chronic Widespread Pain, J Manipulative Physiol Ther 2006;29:493- 501.
[69]Brady, David M. , DC, Michael J. Schneider, DC, A new paradigm for differential diagnosis and treatment, JMPT, Volume 24, Issue 8, Pages 529-541 (October 2001).
[70] Occupational Medicine Practice Guidelines: Evaluation and Management of Common Health Problems and Functional Recovery in Workers, 2nd Edition, 2008 revision.
[71] Millea P & Holloway R, Treating Fibromyalgia , Amer Family Physician – 2000 Oct; 62(7).
[72] Blunt KL, Rajwani MH, Guerriero RC. The effectiveness of chiropractic management of fibromyalgia patients: a pilot study. J Manipulative Physiol Ther 1997;20:389-99.
[73] Keating, Joseph C. Jr., PhD, “The Meanings of Innate,” J Can Chiropr Assoc 2002; 46(1)
[74] Palmer D.D., The Science, Art and Philosophy of Chiropractic. Portland, Oregon: Portland Printing House Company, 1910.
[75] Palmer, ibid. pp. 18-19.
[76] Strang, ibid. pp. 33-35.
[77] Interviewed by David Hirschman, Recorded September 13, 2010, BigThink.com
[78] Interviewed by David Hirschman, Recorded September 13, 2010, BigThink.com
[79] Stephen Hawking, Colbert Report: 9/16/10.
[80] Hadler, NM, Stabbed in the Back; confronting back pain in an overtreated society, University of North Carolina Press, 2009, pp. 64
[81] http://thinkexist.com/quotes/morris_fishbein/
[82] Ibid. p. 493.
[83] Neuburger, M. (1944) “An Historical Survey of the Concept of Nature from a Medical Viewpoint” Isis 35 (1): 16–28
[84] Medical Guesswork, From heart surgery to prostate care, the health industry knows little about which common treatments really work, Business Week, May 29, 2006
[85] Welling & Company and the Oklahoma chiropractic research foundation in cooperation with the chiropractic association of Oklahoma in 1984 that surveyed the “attitudes toward chiropractic health care in Oklahoma”
[86] Kaptchuk Ted J., OMD, and David M. Eisenberg, MD The Persuasive Appeal of Alternative Medicine, Annals of Internal Medicine, 15 December 1998 | Volume 129 Issue 12 | Pages 1061-1065
[87] Keating, JC, Toward a Philosophy of the Science of Chiropractic, 1992, pp. 30.
[88] Palmer, DD, ibid. p. 495.
[89] Gromala, Theresa, “Broadsides, Epigrams, and Testimonials: The Evolution of Chiropractic Advertising,” 1984 Chiropractic History, 4(1): 40-45.
[90] 1951 (May 15): letter from BJ Palmer to “Dr. Marchus Bach,” School of Religion, State University of Iowa, Iowa City IA
[91] Palmer BJ. Giant versus pygmy. A portion delivered at the 47th Annual PSC Lyceum and Homecoming, 1959. Palmer School Chiropractic: Davenport; 1959
[92] Hadler NM. The last well person. Montreal: McGill-Queen’s University Press (in press).
[93] Evidence-Based Medicine or Faith-Based Medicine? Medscape Posted 12/10/2004.
[94] Action Digest. American Chiropractic Association. January, 1977. Quoted from The Journey of Scott Haldeman by Reed B. Phillips.