Bitter Pill: Part 2
The recent TIME magazine (March 4, 2013) cover story, “Bitter Pill: Why Medical Bills Are Killing Us”, by attorney/journalist Steven Brill discusses how badly the medical system is broken: most importantly, why it is so expensive considering the U.S. spends more on healthcare than the next ten highest spending countries combined.
In a recent interview on The Daily Show with Jon Stewart, Mr. Brill mentioned that Obamacare addressed one important question: the need to cover the costs of these huge medical bills that are literally bankrupting this country.
In his exposé, Mr. Brill addresses a second question: “No one asked why these bills were so high.”
“Put simply, with Obamacare we’ve changed the rules related to who pays for what, but we haven’t done much to change the prices we pay. When you follow the money, you see the choices we’ve made, knowingly or unknowingly.”[1]
As he found, following the medical money trail is an uphill battle, similar to looking for the Holy Grail. Unbeknownst to patients, there are not only many costs hidden in medical/hospital bills as Mr. Brill revealed, but there are many ineffective medical treatments that remained off his investigative radar that add to the burden of healthcare costs.
These costs are a growing problem that people fail to understand. To put the current 2.8 trillion dollar healthcare cost into perspective, the U.S. spent twice as much on medical care as it did on food in 2006—and more than China’s 1.3 billion citizens consumed altogether.
In addition, the increase in U.S. healthcare spending in the three-year period of this study is more than the amount U.S. consumers spent on oil and gasoline during all of 2006 when energy prices began to reach new heights.[2]
Certainly these astronomical medical costs are potentially mortal to our economy as President Obama and Mr. Brill have noted, but may I suggest there are two more essential questions that need to be asked:
1) How well do medical treatments actually work, and
2) Are they all really necessary?
The chiropractic profession has asked these two questions in regards to spine care for over twenty years but has been ignored by the medical profession and a medically-biased media. After all, for the $2.8 trillion Americans spend on healthcare, we should have the healthiest society on the planet, but we certainly don’t.
Question #3: Is Medical Care Effective?
While President Obama and Mr. Brill are concerned about health insurance coverage and high medical costs, they ignore another fundamental question concerning the effectiveness of medical care.
The Washington Post published a recent article to this effect: “Surprise! We don’t know if half our medical treatments work” by Sarah Kliff who reported on an article in the British Medical Journal.
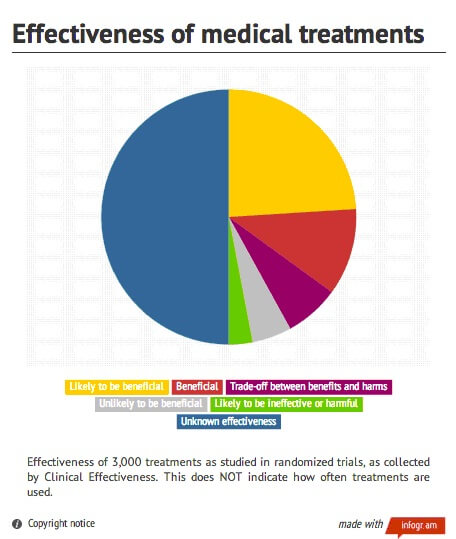
The following pie chart is shocking considering it shows nearly 2,000 of 3,000 medical treatments studied fall into these categories:
“Unlikely to be beneficial”,
“Likely to be ineffective or harmful”,
a “Trade-off between benefits and harms”, and
half are of “Unknown effectiveness.”
As one example of ineffective medical care, the recent 60-minute exposé, Deadly Dose, on CNN by Dr. Sanjay Gupta (November 18, 2012), focused on the 37,000+ deaths from narcotic painkillers like OxyContin. About 21,000 involved prescription drugs and of those 75 percent were pain killers taken for chronic back pain.
President Clinton asked him to do this after the son of one of his supporters died unexpectedly from OxyContin mixed with alcohol. He also called for a “national discussion” to solve this growing problem of prescription drug addiction.
Ostensibly, the viewers were led to think in this hour-long program that Dr. Gupta was seeking a non-drug solution to this epidemic of back pain, but he omitted any reference to the most obvious, proven, and effective non-drug treatment, chiropractic care.
Indeed, many viewers, such as the twenty million chiropractic patients and 80,000 chiropractors like me, must have been perplexed how any journalist can speak of non-drug back pain treatments and not mention chiropractic care.
His professional amnesia typifies the present medical mindset that opposes open competition in a free market. Simply put, Dr. Gupta has no incentive to see the spine surgeon’s money trail detoured to chiropractors, even it if might avoid deadly addictions and save many lives.
As a neurosurgeon, Dr. Gupta knows back surgery is big business. The average annual salary of a spine surgeon is now the highest paid of all doctors at $806,000 according to Bloomberg News.[3] This salary does not include the royalties and commissions paid by surgical hardware manufacturers that often top the million dollar level as The Wall Street Journal revealed in an article, “Top Spine Surgeons Reap Royalties, Medicare Bounty.”[4]
Dr. Gupta obviously has a conflict of interest as a journalist who has no interest to endorse his profession’s primary competition for spine cases—those pesky chiropractors who are now recommended by every international guideline on back pain treatments, a fact he has never mentioned on CNN.
Mr. Brill spoke of this point—the lack of free enterprise in healthcare—in his lengthy 36-page exposé:
“It’s about facing the reality that our largest consumer product by far—one-fifth of our economy—does not operate in a free market…
“We’ve created a secure, prosperous island in an economy that is suffering under the weight of the riches those on the island extract. And we’ve allowed those on the island and their lobbyists and allies to control the debate…”[5]
I might add the medical media is an “ally” that controls this debate as we’ve seen with Dr. Gupta’s biased reporting that excludes chiropractic care as a viable option to drugs, shots, and spine surgery. Obviously the huge compensation to back surgeons is one glaring example of the “prosperous island” that Mr. Brill mentions.
CNN and Dr. Gupta are not alone as “allies” who control this debate by boycotting chiropractic in the news.
National Public Radio (NPR) also has developed a bad case of amnesia. Accounting by Highbeam.com shows only 13 articles on chiropractic in 185,069 segments on NPR programs that equates to a frequency rate of only 0.0070091%.[6]
Considering the fact that the chiropractic is the third-largest physician-level profession in the world, the scarcity of accurate news coverage is appalling during the present pandemic of back pain, now considered the #1 disabling condition worldwide.
Indeed, if there are glaring mistakes in Obamacare, it was not breaking up the medical cartel or demanding a Fairness Doctrine in the media reporting on alternatives to medical care. Without good choices, patients are doomed to the same old medical methods that have gotten America into this present healthcare dilemma.
Mr. Brill spoke of this “perverse motivation” among doctors and in hospitals; “When you follow the money, you see the choices we’ve made, knowingly or unknowingly.”
This is most evident with treatments for the epidemic of back pain. For example, why would a hospital knowingly want chiropractic care available when a spine surgery patient brings in ten times more revenue for the same diagnostic case of low back pain?
As Mr. Brill indicated in his report, hospitals are notorious for over-use of tests and treatments, which is most obvious with the increasing amount of expensive and harmful medical spine practices.
I might add hospitals are notorious for discrimination against chiropractors and all CAM providers that are cheaper, safer, and often more effective than drugs, shots, and surgery.
Despite the evidence supporting CAM methods for back pain (principally Chiropractic, Acupuncture, and Massage therapy), from 1994 to 2007, JAMA reported the patient population increased by only 12%, but MRIs increased 307%, spinal fusion surgery increased 204%, spinal injections increased 629%, and opiate use increased 423%.[7]
Without question, the medical profession has knowingly ignored the paradigm shift in spine care that has refocused attention on CAM treatments over medical spine care for the 85% of mechanical low back cases, which means the problem is patho-physiological, not patho-anatomical. In other words, joint dysfunction is the cause of most back problems rather than the 15% of those cases caused cancer, fractures, infections or true disc ruptures that require medical care.
The seminal research in spine care essentially began in 1990 when MRI research by Scott Boden, MD, now director of the Spine Center at Emory University, debunked the discogenic theory when he found many people without back pain also had herniated or degenerated discs.[8]
Richard Deyo, MD, MPH, also agreed that “many of these disc abnormalities are trivial, harmless, and irrelevant, so they have been dubbed incidentalomas,” equivalent to “finding gray hair” since both are part of the normal aging process.[9]
Despite this research undermining the “bad disc” theory that still permeates in medical practices, spinal fusion costs covered by Medicare escalated to $2.24 billion in 2008—nearly a 400% increase in cost since 1997.[10]
Spine researchers also admit to the tsunami of MRI imaging tests and medical treatments of drugs, shots, and surgery:
Narcotic painkillers in 2010 killed 38,329 people (more than deaths from illicit drugs) of whom 75% were taking for back pain;
Spinal injections have been deemed no more effective than placebo and recently attributed to deaths from meningitis infections;
MRI scans are detecting anatomical disorders chided as “incidentalomas” because “bad discs” are often incidental to the patients’ pain; and
Back surgeons have gone wild “leaving more tragic human wreckage in its wake than any other operation in history.”[11]
Dr. Boden also admitted, “Many, if not most, primary medical care providers have little training in how to manage musculoskeletal disorders.”[12]
These examples explain why Mark Schoene, editor of THE BACKLetter, an international spine research newsletter from Georgetown University, also criticized the ineffective medical spine methods when he stated, “Spinal medicine in the US is a poster child for inefficient spine care.”[13]
Question 4: Are All Surgeries Necessary?
Not only is medical care and hospitalization incredibly expensive as Mr. Brill’s TIME article clearly shows, it is also inefficient when two-thirds of medical care is considered ineffective as the recent British Medical Journal study revealed.
But another important question Mr. Brill did not broach is whether or not all surgeries are actually necessary considering the huge number performed. Indeed, the numbers are astounding compared to other countries with better health statistics. Indeed, no other country does nearly as many operations on its citizens.
In 2006, American doctors performed at least sixty million surgical procedures of all types, one for every five Americans. Over hundred thousand people die each year from complications of surgery—far more than die in car crashes; deaths from prescription drugs now ranks fourth only to cancer, heart disease, and diabetes, and when added to deaths from botched surgery, over 3,000 Americans die weekly.[14]
The Dartmouth Institute of Health Policy also in 2006 suggested 30-40% of spine, heart, knee, and hip surgeries (and the associated hospitalization costs) were unnecessary.[15] Yet there is no sign these unnecessary surgeries are slowing down.
Certainly hospitals prefer the most expensive procedures, most commonly heart and back surgeries. Yet patients are rarely told there are alternative treatments to avoid these costly, disabling, and often deadly procedures.
By law, however, doctors are required to acquire informed consent from patients, which means they are to be told two things after the exams and before treatment begins. First, the doctor is legally required to tell them the proposed treatment and possible risks and, secondly, the patient is to be informed of alternative treatments and risks.
Often patients are not told chiropractic care is a recommended option to medical care for the majority of back pain cases. Instead, they are frightened by unethical surgeons who tell them chiropractic care might paralyze them, a lie every chiropractor has heard many times.
The fact is malpractice insurance companies know who’s hurting patients since they pay the claims, and the actuaries show that chiropractors have the lowest malpractice rates among all spine practitioners. Chiropractors pay approximately $1,600 annually[16] compared to spine surgeons, who typically will pay approximately $71,000 to over $200,000,[17] which clearly suggests the safety of care provided by chiropractors.
Considering 40% of spine surgeries are considered unnecessary by Dartmouth, if chiropractic care were utilized as the first avenue of care for the 85% of non-specific mechanical low back cases as the guidelines recommend, this could save billions of dollars as well as help millions of patients avoid potential disability from failed back surgery, drug dependency, and additional medical costs.
Many experts believe the cost of medical care will be reduced substantially when unnecessary spine surgeries are avoided along with the costs associated with chronic disability, lost wages, and future treatments.
Considering the estimated cost of back pain is $267.2 billion annually[18], a 40% reduction would save $106 billion, which is equivalent to the cost of the war in Afghanistan for one year.[19]
Pandemic of Pain
The enormity of back pain and the benefits from chiropractic care are facts most people fail to realize due to the medical media boycott of all things chiropractic as we’ve witnessed on CNN and NPR.
Musculoskeletal conditions such as low back pain, neck pain, and arthritis affect more than 1.7 billion people worldwide. Low back pain has become the number-one cause of disability worldwide and neck pain the number-four cause. Overall, musculoskeletal conditions represent the second leading cause of global disability.[20]
According to Scott Haldeman, MD, DC, PhD, a leading inter-professional spine expert: “Spinal disorders have a greater impact than HIV/AIDs, malaria, lower respiratory infections, stroke, breast and lung cancer combined, Alzheimer’s disease, diabetes, depression or traffic injuries.”[21]
Dr. Haldeman’s study found back pain is virtually inescapable considering it will strike most of the 250 million American adults sometime in their lifetime.[22]
Nearly one-third of adults will suffer daily with low back pain, which equates to 92.5 million people;
two-thirds of adults will have a back attack within the year, which equates to 190 million;
85% or 212.5 million adults will have a severe back attack in their lifetime, and
20% will describe their pain as severe and crippling.[23]
When low back pain is combined with neck pain, these painful spinal disorders are second only to ischemic heart disease in its impact on the global burden of disease according to Dr. Haldeman.
This is yet another way the 80,000 chiropractors, who today constitute the third-largest, physician-level health profession in the country, could improve this dire U.S. disadvantage with their superior diagnostic and clinical skills in spine care as America’s primary spine care providers.[24]
This is not new information. As far back as 1993, health economist Pran Manga, PhD, showed in his comparative studies that chiropractic care could save billions and help millions of patients with spine-related disorders. “There is an overwhelming body of evidence indicating that chiropractic management of low back pain is more cost-effective than medical management.”[25]
By 1994, the US Public Health Service’s Agency for Health Care Policy and Research (AHCPR) issued its 14th guideline, a 170-page study entitled “Acute Low Back Pain in Adults.”[26] Its findings also confirmed the rare need for surgery (1 in 100 cases) except in the most severe cases (fractures, cancer, serious infections, or cauda equina). Moreover, spinal manipulation was recommended as a “proven treatment.”
Despite these formal studies that recommended chiropractic’s brand of spine care—spinal manipulative therapy—after the AHCPR study, the “back surgeons went wild” according to author Shannon Brownlee:
“But when the AHCPR’s panel concluded that there was little evidence to support surgery as a first-line treatment for low back pain, and that doctors and patients would be wise to try nonsurgical interventions first, back surgeons went wild.” [27]
This exemplifies the proverbial 800-pound gorilla in healthcare—a medical monopoly that has fought tooth and nail against any and all competition with different ideas that might allow for a better mousetrap at a cheaper price.
To answer Mr. Brill’s question that “we haven’t done much to change the prices we pay,” one obvious solution for the costly epidemic of back pain is to follow the guidelines that call for chiropractic and CAM methods for the majority of back pain cases.
Certainly having a free market that includes unfettered access to chiropractic care in every public hospital, every workers’ comp program, the military health services, VA programs, Medicare, and group health insurance programs would greatly decrease the high cost of medical spine care by offering a cheaper, safer, and better treatments to the pandemic of chronic back pain.
Yet chiropractic care remains marginalized, “suffering under the weight of the riches those on the island extract,” as Mr. Brill suggests.
Chiropractors remain handcuffed where they are included and discriminated by the AMA’s “wither on the vine” policy adopted after its “contain, eliminate, and destroy chiropractic” strategy was found in 1987 to be in violation of antitrust law in the Wilk et al. v. AMA et al. case.[28]
Unfortunately, the previously open medical warfare simply became a persistent cold war after its defeat in the courtroom.
Although the medical profession has turned a deaf ear to the research evidence in spine care to protect its market dominance, some insurance payers are now listening to the researchers.
In 2011, North Carolina Blue Cross/Blue Shield announced it will no longer pay for spine fusion if the sole criterion is an abnormal disc.[29] Apparently this insurance payer is following the money trail and now wants a detour.
Another recent positive policy change concerning chiropractic care for chronic low back pain occurred when the University of Pittsburgh Medical Center Health Plan announced as of January 1, 2012 candidates for spine surgery must include verification that the patient has “tried and failed a 3-month course of conservative management that included physical therapy, chiropractic therapy, and medication.”[30]
These changes are certainly steps in the right direction, but one that will be resisted by the mainstream spine surgery community and political medicine.
Indeed, if the medical profession is dedicated to evidence-based standards as it proclaims to be scientific, one would think improving the unscientific and ineffective nature of medical spine care should be at the forefront.
Instead, political medicine has waged for over a century a red-herring war against chiropractors and other CAM professionals to deny patients a freedom of choice in healthcare. This medical inquisition attacking CAM methods remains evident today when the AMA’s House of Delegates recently voted to repeal Section 2706 in Obamacare, the non-discrimination clause that would cover CAM treatments and give patients a freedom of choice.
As Mr. Brill found, the era of high tech medical care with advanced imaging, “wonder drugs” and “heroic surgery” has simply not panned out as clinically or cost-effective solutions to American healthcare problems. Instead, this brand of healthcare has created the U.S. health disadvantage that has nearly bankrupted our country while our citizens lead the world in every category of disease.
Without a doubt, the core of this huge healthcare problem can be laid at the doorstep of the AMA itself—the “prosperous island” as Mr. Brill characterized the medical cartel that unquestionably has become the foremost hindrance to free enterprise, diversity, and progress in healthcare.
As Mr. Brill concluded:
“Over the past few decades, we’ve enriched the labs, drug companies, medical device makers, hospital administrators and purveyors of CT scans, MRIs, canes and wheelchairs. Meanwhile, we’ve squeezed the doctors [including chiropractors] who don’t own their own clinics, don’t work as drug or device consultants or don’t otherwise game a system that is so gameable. And of course, we’ve squeezed everyone outside the system who gets stuck with the bills.”
It is past time to break up the medical monopoly just as the government broke up Standard Oil, AT&T, and Microsoft’s domination of those markets. It is time to allow a free marketplace of complementary and alternative healthcare providers play in this game to give patients something they have not had—access to effective care and freedom of choice based on informed decisions.
JC Smith, MA, DC, is a 33-year practicing chiropractor, author of The Medical War Against Chiropractors, and he maintains a website, Chiropractors for Fair Journalism.
[1] Steven Brill, Bitter Pill: Why Medical Bills Are Killing Us, TIME, Feb. 20, 2013
[2] Diana M. Farrell, Eric S. Jensen, and Bob Kocher, “Accounting for the Cost of U.S. Health Care: A New Look at Why Americans Spend More,” McKinsey Global Institute, November 8, 2008.
[3] Peter Waldman and David Armstrong, “Highest-Paid U.S. Doctors Get Rich with Fusion Surgery Debunked by Studies” Bloomberg News, Dec. 30, 2010.
[4] John Carreyrou and Tom McGinty, “Top Spine Surgeons Reap Royalties, Medicare Bounty,” Wall St. Journal, Dec. 20, 2010
[5] Steven Brill, Bitter Pill: Why Medical Bills Are Killing Us, TIME, Feb. 20, 2013
[6] http://www.highbeam.com/publications
[7] Martin BI, Deyo RA, Mirza SK et al. Expenditures and health status among adults with back and neck problems. JAMA 2008; 299: 656-64
[8] SD Boden, DO Davis, TS Dina, NJ Patronas, SW Wiesel, “Abnormal Magnetic-Resonance Scans Of The Lumbar Spine In Asymptomatic Subjects: A Prospective Investigation,” J Bone Joint Surg Am. 72 (1990):403–408.
[9] RA Deyo and DL Patrick, Hope or Hype: The Obsession with Medical Advances and the High Cost of False Promises (2002):191.
[10] John Carreyrou and Tom Mcginty, Top Spine Surgeons Reap Royalties, Medicare Bounty, WSJ, December 20, 2010
[11] G Waddell and OB Allan, “A Historical Perspective On Low Back Pain And Disability, “Acta Orthop Scand 60 (suppl 234), (1989)
[12] S Boden, et al. “Emerging Techniques For Treatment Of Degenerative Lumbar Disc Disease,” Spine 28(2003):524-525.
[13] The BACKPage editorial vol. 27, No. 11, November 2012.
[14] Atul Gawande, “The Cost Conundrum,” The New Yorker magazine, June 1, 2009.
[15] Elliott Fisher, MD, on the CBS Evening News, “Attacking Rising Health Costs,” June 9, 2006.
[16] National Chiropractic Mutual Insurance Company rate (2009)
[17] The Burton Report, “Why Spine Care is at High Risk for Medical-Legal Suits,” www.burtonreport.com/infforensic/MedMalSpCommonCause.htm
[18] The Burden of Musculoskeletal Diseases in the United States Bone and Joint Decade, Copyright © 2008 by the American Academy of Orthopaedic Surgeons. ISBN 978-0-89203-533-5, pp. 21.
[19] http://www.infoplease.com/ipa/A0933935.html
[20] Peter W. Crownfield, Back Pain Is #1 Cause of Disability Worldwide, Global Burden of Disease 2010 highlights the pressing need to prevent, treat spinal and musculoskeletal disorders. Dynamic Chiropractic – February 15, 2013, Vol. 31, Issue 04
[21] Scott Haldeman, Analysis of Global Burden of Disease Study 2010 Impact of Spinal and MSK Disorders
[22] The Burden of Musculoskeletal Diseases in the United States Bone and Joint Decade, Copyright © 2008 by the American Academy of Orthopaedic Surgeons. ISBN 978-0-89203-533-5, pp. 21.
[23] Scott Haldeman DC, MD, PhD, FRCP(C) and Simon Dagenais DC, PhD. A supermarket approach to the evidence-informed management of chronic low back pain. The Spine Journal, vol. 8, Issue 1, January-February 2008, Pages 1-7.
[24]Donald R Murphy, Brian D Justice, Ian C Paskowski, Stephen M Perle, Michael J Schneider, The Establishment of a Primary Spine Care Practitioner and its Benefits to Health Care Reform in the United States, Chiropractic & Manual Therapies 2011, 19:17
[25] P Manga, D Angus, C Papadopoulos, W Swan, “The Effectiveness and Cost-Effectiveness of Chiropractic Management of Low Back Pain,” (funded by the Ontario Ministry of Health) (August, 1993):104
[26] Bigos et al. US Dept. of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research, Clinical Practice Guideline, Number 14: Acute Low Back Problems in Adults AHCPR Publication No. 95-0642, (December 1994)
[27] S Brownlee, “Newtered,” Overtreated: Why Too Much Medicine Is Making Us Sicker and Poorer, http://overtreated.com/extras01.html
[28] Chester A. Wilk, James W. Bryden, Patricia A. Arthur, Michael D. Pedigo v. American Medical Association, Joint Commission on Accreditation of Hospitals, American College of Physicians, American Academy of Orthopaedic Surgeons, United States District Court Northern District of Illinois, No. 76C3777, Susan Getzendanner, Judge, Judgment dated August 27, 1987
[29] www.bcbsnc.com/assets/services/public/pdfs/medicalpolicy/lumbar_spine_fusion_surgery.pdf
[30] Crownfield, Peter W., “Chiropractic Before Spine Surgery for Chronic LBP,” Dynamic Chiropractic, vol. 30, no. 11, May 20, 2012.