February 25, 2014
Risa Lavizzo-Mourey, MD, MBA
President and Chief Executive Officer
The Robert Wood Johnson Foundation
RE: My View of Your Bird’s Eye View
Dear Dr. Risa:
I read with great interest your hopeful message, Building a Culture of Health. I found it to be a very astute treatise concerning the “human condition” in healthcare today, certainly a dire situation for all Americans.
But may I ask: does your invitation include chiropractors?
I ask this knowing full well the long-standing antipathy by mainstream medicine toward my profession. In fact, I recently authored The Medical War Against Chiropractors examining the “chiropractic condition” in healthcare, if you will.
Dr. Risa, you may understand such discrimination firsthand knowing that many women have hit glass ceilings in the corporate world, overlooked by virtue of their gender, and underpaid for equivalent services as female executives in a male-dominated world.
Regrettably, the situation for chiropractors in health care is a similar but untold story of struggle for equality. Like racism or sexism, medical prejudice is steeped in misguided beliefs. Just as the n-word and b-word have no place in our egalitarian society, nor does the q-word belong in healthcare, an epithet long used by MDs to denigrate chiropractors.
Long before any substantial improvement can occur, I believe tolerance must be a focal point in your equation to improve the American healthcare system. Without diversity and equality, America cannot change as it needs to do.
Before I address your commentary, “A Bird’s Eye View,” please let me preface my notion how to build a culture of health, particularly in regards to spine care, an issue mired in many controversies.
“Chiropractic Must Die”
Dr. Risa, let me ask you a simple question: when was the last time you’ve seen an informative, in-depth, fair, and balanced program about chiropractic care on national TV? If like most people, probably never.
Indeed, the chiropractic profession remains missing in the media due to a lingering bias that is not by chance but the result of a massive and lengthy AMA-sponsored campaign to disparaged chiropractors.
Although racism, sexism, and anti-Semitism have unknown origins, the stigma against chiropractors can be traced back to one man, Morris Fishbein, MD, CEO of the AMA from 1924 to 1949. Due to his tyrannical leadership, he was dubbed the “Medical Mussolini” by his contemporaries.[1]
Beginning in the 1930s, Fishbein made his goal perfectly clear:
“Eight years ago [in 1932] officials of the American Medical Association met in secret conclave in Chicago and adopted the slogan ‘Chiropractic must die.’ They gave themselves ten years in which to exterminate it.”[2]
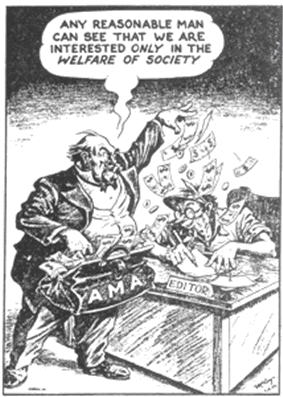
Fishbein’s defamation campaign later continued from 1962 to 1980 by the AMA’s Committee on Quackery whose clandestine tactics included using third-party writers, including columnist Ann Landers, who would give the appearance that “everybody knows that chiropractic is an unscientific cult”[3] in its campaign to “contain and eliminate the chiropractic profession”[4] that was eventually deemed illegal in federal antitrust court {Wilk et al. v. AMA et al.}[5].
The Court also ordered a permanent injunction against the AMA due to “lingering effects of the illegal boycott and conspiracy”… “injury to chiropractors’ reputations,” and “economic injury as a result of the boycott.”
However, the public has never been told of this illegal ploy to impugn chiropractors or that the source of this stigma came from an organized campaign of defamation by the AMA, not from governmental agencies, licensing boards, or from the public at large.
Indeed, this media meddling remains off the public’s radar. To this day, many people still parrot the old medical propaganda without realizing its source. Like erasing the vestiges of racism, this medical prejudice will take time to undo because the bias in the media continues today.
For example, when I researched the frequency of chiropractic as a topic on my six favorite NPR programs, I was startled to find only 13 articles on chiropractic in 185,069 segments that equates to a frequency rate of only 0.007%. The news program All Things Considered produced only 8 of 87,252 segments since 1990 (0.009%), revealing NPR does not “consider all things” when it comes to chiropractic care.
It is terribly disturbing when the most progressive public radio network fails to consider the benefit chiropractors bring to the table in healthcare reform that could help millions and save billions. Apparently the media has developed a bad case of “professional amnesia” by ignoring the ascendancy of chiropractic care during this back pain epidemic as the research has now shown.[6]
Even the Robert Wood Johnson Foundation may be accused of professional amnesia about chiropractic. While searching for “back pain” at the RWJF website, I found 86 hits, but only two contained the word “chiropractic” in only a passing regard.
Obviously there is a need to end this lingering ignorance about the benefits of chiropractic care if we are to help this pandemic of back pain. It’s past time to shed new light on this old problem.
The Burden of Back Pain
The call for reform in spine care is massive today considering back pain is the #1 disabling condition in the world that will affect 90% of Americans during their lives.
A continuing flurry of news articles has revealed the abuse, expense, and “inefficient” nature of medical spine care (opioids, ESIs, and fusions).
The following is a short list of recent news articles critical of medical spine care:
- “Highest-Paid U.S. Doctors Get Rich with Fusion Surgery Debunked by Studies” by Peter Waldman and David Armstrong, Bloomberg News, Dec. 30, 2010
- “Surgery May Not Be the Answer to an Aching Back,” by Joanne Silberner, NPR, April 6, 2010
- “Why You Should Never Get Fusion Surgery For Plain Back Pain” by Robert Langreth, Forbes, Jan. 10, 2011
- “600,000 Americans have back surgery each year,” TODAY, September 11, 2012
- Study Says Back Surgery Often Makes Things Worse, The Daily Hit, Oct 14, 2010
- “New Study Reveals That Back Surgery Fails 74% of the Time,” [7] SPINE 2011 (Feb 15);36 (4):320–331
- “Back Pain Eludes Perfect Solutions” by Leslie Berger, The New York Times, May 13, 2008
- “Epidural steroid shots debated amid meningitis scare,” USA Today, Oct 6, 2012
- “Opioid Painkiller Prescriptions Pose Danger Without Oversight,” Barry Meier, The New York Times, April 8, 2012
- “Back Surgery May Backfire on Patients in Pain,” by Linda Carroll, MSNBC.COM, Oct. 14, 2010
- “Top Spine Surgeons Reap Royalties, Medicare Bounty,” by John Carreyrou And Tom McGinty, Wall St. Journal, Dec. 20, 2010
- “Medicare Records Reveal Trail of Troubling Surgeries” by John Carreyrou and Tom McGinty, Wall St. Journal, March 29, 2011
- “How Back Pain Turned Deadly” by Elisabeth Rosenthal, The New York Times, November 17, 2012
- “Fee-for-service rewards volume: Our view” The Editorial Board, USA TODAY, July 7, 2013
- “Back pain: Doctors increasingly ignore clinical guidelines,” The LA Times, July 29, 2013
- “Patients with back pain often get the wrong treatment,” USA Today, July 29, 2013
- “Worrisome Trends in Back Pain Management,” Medscape Medical News, July 30, 2013.
- “New solutions for long-lingering back pain – CBS News,” CBS This Morning, July 31, 2013.
- “Former Hospital CEO, Calif. Senator Charged in Insurance Fraud Case,” California Healthline, Feb. 24, 2014
- “Outpatient Back Pain Treatments: Not What the Doctor Should Order,” by Jaime Toro, MD, The New England Journal of Medicine, August 20, 2013
- “The Back Pain Most Surgeons Won’t Find,” by Dr. Nick Shamie, CNN.com, September 18, 2013
- “Hospital Executive Pleads Guilty in Bribes Case,” by John Carreyrou, WSJ, Feb. 21, 2014
Such investigations come as no surprise considering back pain is a $300 billion industry in the US alone ($600 billion worldwide) that equates to 10% of the total $3 trillion US healthcare expense.[8]
The impact of back pain is enormous according to Dr. Scott Haldeman, DC, MD, PhD, adjunct professor at UCLA:
“Spinal disorders have a greater impact than HIV/AIDs, malaria, lower respiratory infections, stroke, breast and lung cancer combined, Alzheimer’s disease, diabetes, depression or traffic injuries.”[9]
Dr. Haldeman served on the US Public Health Service’s Agency for Health Care Policy & Research (AHCPR) Clinical Guidelines Committee on Acute Low Back Problems in Adults as well as presided over The Bone and Joint Decade 2000 to 2010 Task Force on Neck Pain and Its Associated Disorders.
He confirms that every credible guideline on spine care now recommends conservative care first:
“The paradigm shift has already taken place. Non-surgical, non-invasive care is already the first choice for treatment for spinal disorders in the absence of red flags for serious pathology in virtually all guidelines.”[10]
Many renowned spine experts are also speaking out on the paradigm shift in spine care. In fact, some suggest this huge burden can be laid at the doorstep of medical spine care (opioid drugs, epidural shots, fusion surgery) that has been dubbed the “poster child of inefficient spine care” by Mark Schoene, associate editor of THEBACKLETTER, a leading international spine research journal.
Mr. Schoene also warns that “such an important area of medicine has fallen to this level of dysfunction should be a national scandal. In fact, this situation is bringing the United States disrespect internationally.”[11]
Mr. Schoene’s analysis reflects the growing consensus among spine researchers nowadays. Despite the increasing scientific studies and newspaper articles exposing the overall ineffectiveness of medical spine care as well as the corruption in the spine surgery field, most people remain unaware of this paradigm shift to conservative care.
So the obvious question remains: why is back pain the #1 disabling condition in the world?
With shameless audacity, I daresay the evidence shows the medical war on chiropractic is the most logical explanation by suppressing what is now considered a “proven treatment.”[12]
Imagine if the AMA had waged a war on dentists how bad Americans’ dental health would be today. Of course, our smiles would be very poor if the AMA had conducted a similar boycott of dentists as it did against chiropractors.
Building Bridges: A Chiropractic Response
With these facts in mind, Dr. Risa, please allow me now to address your commentary, “A Bird’s Eye View,” where I saw a glimpse for hope for progress when you wrote:
- “What new bridges must our Foundation help build to make a culture of health part of the grander whole of what it means to be an American?”
Before the RWJF can build “new bridges” or implement new strategies, it is imperative to rebuild those bridges burned by the AMA in is quest of a monopoly position as well as rebuke medical strategies shown to be ineffective as the Washington Post revealed, “Surprise! We don’t know if half our medical treatments work” that reported on an editorial in the British Medical Journal.
I believe the obvious answer to “the grander whole of what it means to be an American” is that of inclusion, diversity, equality, and not what we’ve seen in the present segregated and monopolistic American healthcare system. Considering only 2% of PCPs refer to chiropractors, obviously there is a huge need to build a bridge of respect by medical primary care practitioners toward chiropractors.[13]
The bottom line is clear: a medical mea culpa is essential before a healthcare tabula rasa can proceed to improve the health of all Americans.
Historically, the call for healthcare equality initially began with Dr. Benjamin Rush, a Founding Father and Signer of the Declaration of Independence, who warned of the rise of a “medical monarchy.” Dr. Rush, regarded as the father of American medicine, believed in the separation of powers as it applied to the exercise of the professions. He wrote:
“The Constitution of this Republic should make specific provision for medical freedom as well as for religious freedom. To restrict the practice of the art of healing to one class of physicians and deny to others equal privileges constitutes the Bastilles of our science. All such laws are un-American and despotic. They are vestiges of monarchy and have no place in a republic.” [14]
His call for equality in healthcare is similar to President Obama’s call for building “ladders of opportunity” in his State of the Union address. His theme of inclusion is already a part of the Affordable Care Act, specifically Section 2706, the non-discrimination provision, that prevents insurance companies and health plans from arbitrarily excluding the participation of non-MDs such as doctors of chiropractic.
One of the “new bridges” your Foundation should build is to integrate healthcare disciplines for the betterment of all Americans, but I seriously question if the medical status quo is amenable to equality considering its historically intolerant attitude.
Similar to old Southern racists, integration with any minority runs against the AMA’s grain. In fact, it wasn’t until 2008 that the AMA apologized to black MDs for its history of excluding black physicians from membership, for listing black doctors as “colored” in its national physician directory for decades, and for failing to speak against federal funding of segregated hospitals and in favor of civil rights legislation.[15]
I find a similar situation exists today considering nearly every patient who comes to my office as the proverbial ‘last resort’ should have visited a chiropractor years ago, but were dissuaded by their local intolerant MD who told them, “don’t come crawling back to me after that quack paralyzes you,” who then dispenses addictive opioids like Halloween candy or recommends ineffective epidurals or unnecessary spine surgery.
- “We will work in tandem with others to transform what it means to be a healthy nation. We will amplify the voices calling for change.”
The first official “call for change” in spine care occurred twenty years ago in 1994 when the AHCPR guideline on acute low back pain in adults deemed spinal manipulation a “proven treatment.”[16] In fact, SMT was the only physician-level initial treatment recommended. Other than NSAIDs and hot/cold packs, it did not recommend narcotic drugs, epidural shots, or standard physical therapeutics as typically done today.
Moreover, the panel did not recommend spine surgery:
“Even having a lot of back pain does not by itself mean you need surgery. Surgery has been found to be helpful in only 1 in 100 cases of low back problems. In some people, surgery can even cause more problems. This is especially true if your only symptom is back pain.”[17]
Before the ink had dried, this AHCPR guideline was sabotaged by the North American Spine Society, proving transformation will not happen until the “voices calling for change” in spine care are embraced rather than thwarted by the powerful allies within the medical spine industrial complex—surgeons, hospitals, device manufacturers, MRI centers, and, of course, Big Pharma.
Steven Brill, in his TIME magazine (March 4, 2013) cover story, “Bitter Pill: Why Medical Bills Are Killing Us”, discussed how badly the medical system is broken: most importantly, why it is so expensive considering the U.S. spends more on healthcare than the next ten highest spending countries combined. Mr. Brill called for a change from the “perverse motivation” among doctors and in hospitals: “When you follow the money, you see the choices we’ve made, knowingly or unknowingly.”
This is most evident with treatments for spine care. For example, why would a hospital knowingly want chiropractic care available when a spine surgery patient brings in ten times more revenue for the same diagnostic case of low back pain?
Obviously the inclusion of chiropractic care would be painfully detrimental to the income of the medical spine complex no matter the benefits it would bring by lowering costs for payers and improving outcomes for patients.
Although this paradigm shift in spine care is important to solve this burden of pain, it does little good if the guidelines are not followed by MDs or remain unknown to the public, two problems the RWJF can certainly help to amplify by sponsoring educational programs.
- “Still, we know that building this vision of a culture of health will take time. It will take fortitude. It will take collaboration. And we certainly cannot do it alone.”
It goes without saying that “fortitude” is the backbone of the chiropractic profession. For over a century unlike any other health profession we have endured segregation and slander. While this oppression definitely bowed our backs and thickened our skin, as a result, however, chiropractic has not grown as substantially as it should had this medical apartheid never occurred.
Not only is the medical profession resistant to chiropractic spine care, researchers have found that even today it takes 15 years for a new treatment to be incorporated into mainstream medical practice and, more shocking, it takes 44 years for a method proven to be ineffective, dangerous, or outmoded to be removed from practices.[18]
I agree with you that “this vision…will take time,” but the biggest obstacle will be changing the intransigent attitude of the medical profession.
- “As always, RWJF is committed to realizing this bold transformation through the pursuit of solutions that are evidence-based, measurable, and equitable.”
Let me emphasize strongly that the “evidence-based, measurable, and equitable” solution in spine care is fait accompli as the AHCPR, Dr. Haldeman, Mark Schoene, and other international guidelines have mentioned.
The 1993 meta-analysis by Pran Manga, PhD, health economist, said it best: “There is an overwhelming body of evidence indicating that chiropractic management of low back pain is more cost-effective than medical management.”[19]
The challenge is to enforce the guidelines has already gotten traction by some Medicare Accounting Contractors that refuse to pay for spine fusions if conservative care was not used beforehand. Private insurers such as the North Carolina BC/BS also now mandate conservative care like chiropractic manipulation before drugs, shots, and surgery.
Of course, the medical spine complex is fighting this “pursuit of solutions” just as they fought the original AHCPR guideline in 1994.
- “It means carefully implementing strategies to reduce wasteful spending, while at the same time maintaining or increasing quality.”
If RWJF is committed to “increasing quality,” promoting the role of chiropractors in spine care would help millions of patients and save billions of dollars.
Aside from the ineffectiveness of medical spine care, there are other alarming revelations concerning the mismanagement of back pain by medical general practitioners who have been shown to be “inept” in their training on musculoskeletal disorders,[20] more likely to ignore recent guidelines,[21] and more likely to suggest spine surgery than surgeons themselves.[22]
Unfortunately, such incompetence in musculoskeletal disorders translates into “wasteful spending.” For example, a Washington State workers’ comp study found for patients whose first provider was a chiropractor, only 1.5% had surgery in contrast to 42.7% of workers who went through the typical medical system inevitably had surgery.[23]
Considering in 2006 the Dartmouth Institute of Health Policy[24] suggested 30-40% of spine surgeries (and the associated hospitalization costs) were unnecessary, a 40% reduction in this $300 billion dollar cost equates to a potential $120 billion savings for one fiscal year alone.
- “We will persist in supporting the creation of tools and strategies to achieve the highest quality care at the most affordable cost for both the practitioner and the patient.”
I cannot think of a more logical “strategy to achieve the highest quality [spine] care at the most affordable cost” than to promote chiropractors as the portal of entry as primary spine providers for spine-related disorders, a role deserved by our extensive physician-level musculoskeletal education and proven, cost-effective treatments.
The proof is positive and research studies cannot be clearer that chiropractic now stands at the top of spinal treatments as Anthony Rosner, PhD, testified before The Institute of Medicine: “Today, we can argue that chiropractic care, at least for back pain, appears to have vaulted from last to first place as a treatment option.”[25]
- “We are optimistic that America can and will achieve a culture of health if, together, we make it a national priority. RWJF is committed to working with you to reach this goal, and we welcome you to the journey.”
I hope we can agree that a “national priority” in spine care includes fewer spine fusions, fewer epidural injections, and fewer narcotic pain pills in the fight against back pain by using conservative care first. As Mr. Schoene suggests, “such an important area of medicine has fallen to this level of dysfunction should be a national scandal.”
Chiropractic care today has been scientifically vindicated as the foremost solution to this epidemic. If RWJF “welcomes ‘chiropractors’ to the journey,” the time has come to change public sentiment about our brand of spine care by confronting the medical barriers “to reach this goal.”
Tipping Point in Spine Care
Just as MLK, Jr., dreamed of the day when “little black boys and black girls will be able to join hands with little white boys and white girls and walk together as sisters and brothers,” I have a dream, too, that someday healthcare providers will not be judged by their diplomas or by the political dogma of their predecessors but rather by the help they give to patients.
After all, our mutual enemy should not be each other, but pain and disease. Somewhere in the fray this point has been missed.
I believe the tipping point to overcome prejudice begins when the mainstream media creates cognitive dissonance among the public. We’ve witnessed such re-socialization with the equal rights movements with black Americans, we’ve seen it with feminist issues, and now we’ve seen the sudden change in perception about same-sex marriage in the LBGT communities.
In a similar fashion, a new realization about spine care be the tipping point when the public understands the unjust nature of the medical war against chiropractic care has also hurt them as collateral victims subjected to “inefficient medical spine care.”
Indeed, Dr. Risa, what would you say to a patient disabled from failed back surgery, unable to work, addicted to Oxycodone, subjected to ineffective epidural steroid injections, and living with no hope for a better future all because he was medically misdiagnosed, mistreated, and misinformed about chiropractic care? This bleak scenario happens millions of times annually.
The battle facing chiropractic now is not a need for more scientific justification since the evidence-based guidelines have now been established. Today the foremost barrier is a PR battle in the media to inform the public about the benefits of chiropractic care and the evidence-based guidelines that recommend conservative care before medical spine care.
That is the tipping point America must attain in order to improve the spine health of all people. Indeed, it’s past time for a medical mea culpa and tabula rasa in spine care.
Persecution to Vindication
Lastly, Dr. Risa, you quoted the Crow Indian proverb that declares “you already possess everything necessary to succeed,” and I agree. DCs are prepared to succeed as the portal of entry as primary providers for spine related disorders, just as we have been trained to do for over a century.
Two years ago I submitted a grant request to the RWJF without a response to produce a documentary on these very controversial issues, which made me assume medical antipathy was prevalent at RJWF at that time albeit under a different leadership than you.
You can review my proposal, “The War on Chiropractors: The Call for Reform in Spine Care,” that gives my bird’s eye view of this fascinating yet untold story of chiropractic from persecution to vindication. Certainly I am not a documentary producer, but I do realize something must be done to education the public. I view my proposal as the first stepping stone in that process.
I apologize for the length of my letter to you, but hopefully it will share with you how we chiropractors can help you achieve your goal at RWJF to improve the health of all Americans.
Regards,
JC Smith, MA, DC
www.chiropractorsforfairjournalism.com
[1] JH Donahue, “Morris Fishbein, MD: The ‘Medical Mussolini’ and Chiropractic,” Chiropractic History, 16/1 (1996): 39-48.
[2] Wardwell WI. Alternative medicine in the United States. Soc Sci Med 1994;38:1061-1068. (Citing Reed L. The healing cults. Chap 3, Publ No.16 of the Committee on the Costs of Medical Care, p 5. University Press, Chicago, 1932)
[3] W Trever, “in the Public Interest,” Scriptures Unlimited, Los Angeles, Calif., (1972):1
[4] G McAndrews, “Plaintiffs’ Summary of Proofs as an Aid to the Court,” Civil Action No. 76 C 3777, Wilk, (June 25, 1987) Throckmorton, Howard, Taylor, and Monaghon Deps.
[5] Chester A. Wilk, James W. Bryden, Patricia A. Arthur, Michael D. Pedigo v. American Medical Association, Joint Commission on Accreditation of Hospitals, American College of Physicians, American Academy of Orthopaedic Surgeons, United States District Court Northern District of Illinois, No. 76C3777, Susan Getzendanner, Judge, Judgment dated August 27, 1987.
[6] A Rosner, “Evidence or Eminence-Based Medicine? Leveling the Playing Field Instead of the Patient,” Dynamic Chiropractic, 20/25 (November 30, 2002)
[7] Long-term Outcomes of Lumbar Fusion Among Workers’ Compensation Subjects: An Historical Cohort Study, SPINE (Phila Pa 1976) 2011 (Feb 15);36 (4):320–331
[8] The Burden of Musculoskeletal Diseases in the United States Bone and Joint Decade, Copyright © 2008 by the American Academy of Orthopaedic Surgeons. ISBN 978-0-89203-533-5, pp. 21.
[10] Private communication with JC Smith, 7/10/2013
[11] US Spine Care System in a State of Continuing Decline?, The BACKLetter, vol. 28, #10, 2012, pp.1
[12] Bigos et al. US Dept. of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research, Clinical Practice Guideline, Number 14: Acute Low Back Problems in Adults AHCPR Publication No. 95-0642, (December 1994)
[13] Matzkin E, Smith MD, Freccero DC, Richardson AB, Adequacy of education in musculoskeletal medicine. J Bone Joint Surg Am 2005, 87-A:310-314
[14] ER Booth, History of Osteopathy and Twentieth Century Medical Practice, Cincinnati: Caxton Press, 1905 (1924):312.
[15] Kevin B. O’Reilly, AMA apologizes for past inequality against black doctors, amednews staff, July 28, 2008
[16] Bigos et al. US Dept. of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research, Clinical Practice Guideline, Number 14: Acute Low Back Problems in Adults AHCPR Publication No. 95-0642, (December 1994)
[17] Ibid. p. 12.
[18] Refuting Ineffective Treatments Takes Years, The BACKLetter® 101 23/9 ( 2008)
[19] P Manga, D Angus, C Papadopoulos, W Swan, “The Effectiveness and Cost-Effectiveness of Chiropractic Management of Low Back Pain,” (funded by the Ontario Ministry of Health) (August, 1993):104
[20] EA Joy, S Van Hala, “Musculoskeletal Curricula in Medical Education– Filling In the Missing Pieces, The Physician And Sports Medicine,” 32/11 (November 2004).
[21] PB Bishop et al., “The C.H.I.R.O. (Chiropractic Hospital-Based Interventions Research Outcomes) part I: A Randomized Controlled Trial On The Effectiveness Of Clinical Practice Guidelines In The Medical And Chiropractic Management Of Patients With Acute Mechanical Low Back Pain,” presented at the annual meeting of the International Society for the Study of the Lumbar Spine Hong Kong, 2007; presented at the annual meeting of the North American Spine Society, Austin, Texas, 2007; Spine, in press.
[22] SS Bederman, NN Mahomed, HJ Kreder, et al. In the Eye of the Beholder: Preferences Of Patients, Family Physicians, And Surgeons For Lumbar Spinal Surgery,” Spine 135/1 (2010):108-115.
[23] Keeney BJ, Fulton-Kehoe D, Turner JA, Wickizer TM, Chan KC, Franklin GM., Early Predictors of Lumbar Spine Surgery after Occupational Back Injury: Results from a Prospective Study of Workers in Washington State, Spine (Phila Pa 1976). 2012 Dec 12.
[24] Elliott Fisher, MD, on the CBS Evening News, “Attacking Rising Health Costs,” June 9, 2006.
[25] Testimony before The Institute of Medicine: Committee on Use of CAM by the American Public on Feb. 27, 2003.