Ethical Issues in Spine Care
Issue #1: “Minimally Invasive”
Issue #3: New Research Debunks Disc Theory
Issue #4: “You are making people sick”
Issue #5: Follow the Money or Follow the Evidence?
Despite the fact America remains in the throes of a $2.7 trillion healthcare crisis, the medical spine care establishment for over twenty years has ignored new research and evidence-based guidelines that would improve outcomes and lower the huge profits literally made off the backs of unsuspecting patients.
Without question, such adherence to the guidelines would also disprove the century-long medical defamation and boycott of its main competition—the chiropractic profession.
The proof is positive and research studies cannot be clearer that chiropractic now stands at the top of spinal treatments as Anthony Rosner, PhD, testified before The Institute of Medicine: “Today, we can argue that chiropractic care, at least for back pain, appears to have vaulted from last to first place as a treatment option.”[1]
Indeed, under the public radar there are a multitude of ethical issues surrounding medical spine care that spine researchers and journalists are clamoring about but, for the most part, remain sparsely reported in the media and kept very quiet by the medical cartel.
Let me discuss five such ethical issues in this essay.
Issue #1: “Minimally Invasive”
Recently in Macon, Georgia, a spine surgeon advertised a “minimally invasive” procedure for sacroiliac joint (SIJ) pain, but he failed to mention this procedure consists of inserting two titanium screws in the SIJ. His idea of “minimally invasive” seems equivalent to being “slightly pregnant.”
This has become the newest sales pitch among many spine surgeons who, after decades of claiming the SIJ didn’t move and ignored it since there was no disc to fuse, now they finally admit it is a source of pain in 25% of low back pain cases.
Rather than recommending as the first avenue of treatment as their own guideline states—non-invasive spinal manipulation (SMT) done by Doctors of Chiropractic (DCs) to restore normal joint motion—instead they want to completely immobilize the SIJ with screws, which is contrary to restoring proper spinal motion, the key to a pain-free spine.
In the TV ad showing this spine surgeon in his surgical gown and mask doing this “minimally invasive” arthroscopic surgery, he omitted implanting the screws, but it did show him putting a small band aid on his patient, suggesting his surgery is equivalent merely to a child’s boo-boo.
This deceptive ad was inspired by a recent article @ CNN.com entitled, “The Back Pain Most Surgeons Won’t Find” by Dr. Nick Shamie, President of the American College of Spine Surgery, who spoke of SIJ pain that is often overlooked by MDs. His article also inspired my response, Hammer & Nails, about this new spine scam.
Dr. Shamie referred to a 2005 study, “Sacroiliac Joint Pain: A Comprehensive Review of Anatomy, Diagnosis, and Treatment” by Steven P. Cohen, MD, from Pain Management Divisions at Johns Hopkins Medical Institutions and Walter Reed Army Medical Center.
Apparently Dr. Shamie didn’t expect anyone to read this reference since Dr. Cohen’s study points to the lack of evidence for SIJ fusion:
“In patients with SI joint pain unresponsive to more conservative measures, several investigators have advocated surgical stabilization. Unfortunately, all published reports on SI joint fusion have been small case series or retrospective studies.”[2]
In light of this admission, I contacted the Macon spine surgeon asking if he informed patients first to use SMT done by DCs as the guidelines suggest, but he refused to discuss this issue with a less than complimentary reply.
Indeed, he had the typical chauvinistic attitude “Don’t confuse me with the facts.” So, in response to his stubbornness, I answered him by putting a message on my marquee street sign that you might enjoy.

Since 1990 spine researchers have recognized that most back pain (excluding the 10% of red flags cases like fracture, infection, or cancer) generally has little to do with spinal arthritis or disc herniation/degeneration.
How the spine functions—that is, how it moves, bends, and bears weight—is more important than what it looks like on imaging. The main concern to pain-free function is the result of physiologic issues such as vertebral motor unit mechanics of the 313 spinal joints, core strength, flexibility, and axial compression issues caused by prolong sitting or standing.
This research shift is huge, but presently largely ignored by the medical spine cartel consisting of spine surgeons, hospitals, surgical device manufacturers, imaging centers, and Big Pharma.
A recent report now indicates spinal fusion has increased over 600% over the last ten years and has become one of the most expensive procedures in our healthcare system.[3]
Rick Deyo, MD, MPH, et al. reiterated the large increase in spine surgery in their study, “The most complex type of back surgery has increased dramatically between 2002 and 2007 with a 15-fold increase.”[4]
The amount of money at stake is huge considering spine fusion is the leading surgical procedure by cost according to the Centers for Disease Control and Prevention (CDC) 2011 data:
# 1 – Spinal Fusion @ $11.3 billion
# 2 – Balloon Angioplasty @ $11.0 billion
# 3 – Total Knee Replacement @ $10.4 billion
Obviously there is little desire by spine surgeons or hospitals to curtail the tsunami of spine fusions when over $11.3 billion of revenue is at stake despite the research to the contrary. As well, the spinal devices market is expected to reach $13.5 billion by 2016.[5]
Adding fuel to this fire of controversy, researchers at The Dartmouth Institute for Health Policy and Clinical Practice in 2006 suggested nearly 40% of back, heart, hip, and knee surgeries were unnecessary.[6] If the medical cartel were to follow this advice, it would put a huge dent in their profits.
On the other hand according to Dartmouth, in 2008 chiropractic claims accounted for less than 1/10th of 1% of overall Medicare expenditures at an estimated $420 million,[7] yet the OIG is haranguing chiropractors and their Medicare patients who require over twelve office visits per year or, god forbid, maintenance care that comprise 0.037% of the $11.3 billion spine care costs.
The following graphs of spine fusions in Florida from The Washington Post clearly illustrate this tsunami of spine surgeries[8]:
- Fusions increased 16-fold from 969 in 1992 to 15,599 in 2012.
- Average case cost nearly tripled from $40,996 to $111,662.
- Half of the 15,599 were deemed of questionable necessity.
- Medical device and supplies also rose from $12,548 in 1992 to $50,570 per case in 2012.
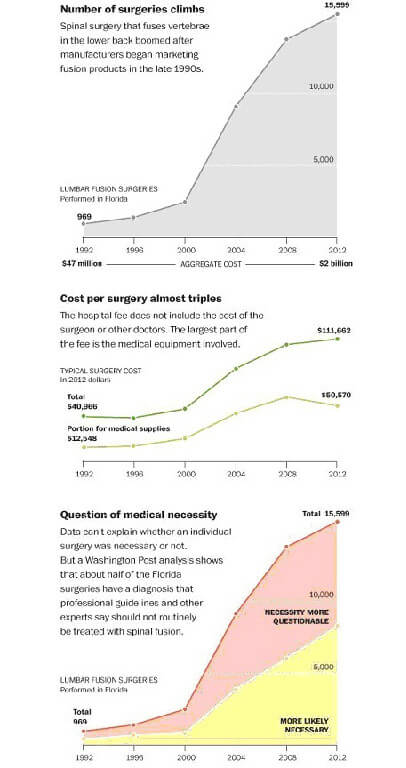
Fusions skyrocketed in 2000 when the FDA approved new devices after a series of studies convinced insurance carriers to pay for them. Little did the FDA foresee fusions were to become the burgeoning cash-cow for spine surgeons, hospitals, and the device manufacturers.
Issue #3: New Research Debunks Disc Theory
Paradoxically, the tsunami of fusions escalated despite the litany of similar studies that followed Scott Boden’s seminal study in 1990 confirming the presence of disc abnormalities in pain-free people.[9]
The AHCPR study in its 1994 guideline #14 on acute low back pain in adults revealed the ugly truth about fusions:
“Even having a lot of back pain does not by itself mean you need surgery. Surgery has been found to be helpful in only 1 in 100 cases of low back problems. In some people, surgery can even cause more problems. This is especially true if your only symptom is back pain.”
“Moreover, surgery increases the chance of future procedures with higher complication rates…There appears to be no good evidence from controlled trails that spinal fusion alone is effective for treatment of any type of acute low back problems in the absence of spinal fracture or dislocations…Moreover, there is no good evidence that patients who undergo fusion will return to their prior functional level.” [10]
Recently a 2013 study from Korea has again debunked the “bad discs” theory when it found as many as 81% of patients had a disc herniation, 89% had an annular fissure, and 95% had evidence of nuclear disc degeneration.[11]
Investigators also found a markedly elevated level of disc abnormalities even among teenagers. “We found close to 25% of [10–19 year-olds] have bulging discs at L5/S1…This increases to nearly 30% [of 20–29 year-olds].” There were also high levels of disc protrusions in those age groups, yet none had back pain. [12]
Another 2013 study from Japan using MRI scans on 975 patients aged 21 to 97 years found the prevalence of disc degeneration over the entire spine was 71% in men and 77% in women younger than 50 years. The prevalence was more than 90% for members of both sexes older than 50 years.[13] Yet none had back pain.
Similarly the other mainstream medical treatments for back pain have also been debunked. Evidence from Johns Hopkins now shows epidural steroid injections (ESIs) are no better than placebo, which is not a new revelation, but one that has also been ignored by pain clinics.[14]
Other research shows that ESIs may actually increase fracture risk. Just a single additional lumbar ESI increases the risk for fracture by 21% and the exogenous use of steroids is the leading cause of secondary osteoporosis according to the results of a large retrospective analysis in an article published in a 2013 issue of the Journal of Bone and Joint Surgery.[15]
Certainly the Hillbilly Heroin epidemic remains rampant as the so-called “pill mills” dispense opioid painkillers like Halloween candy, creating an epidemic of narcotic addiction to the point that Thomas Frieden, MD, director for the CDC, minced no words when he said, “physicians have supplanted street corner drug pushers as the most important suppliers of illicit narcotics.”[16]
Issue #4: Spinal Stenosis Surgery
We now see the same conflict of research vs. reality with the North American Spine Society (NASS) study of lumbar spinal stenosis. With the research trend now critical of spine fusions for “bad discs,” spine surgeons seemingly simply changed their diagnosis.
Since there are always pathoanatomical incidentalomas to be found in older adults to warrant some type of surgery in the minds of spine surgeons, today lumbar spinal stenosis (LSS) has become the leading reason for spine surgery in patients over the age of 65 years.[17]
This NASS guideline mainly focuses on the standard surgical and pharmaceutical treatments, but surprisingly includes a 2006 study of SMT done by DCs for stenosis led by Donald Murphy DC, DACAN, Clinical Director, Rhode Island Spine Center.
Dr. Murphy is now involved with the Primary Spine Provider Network, LLC, to train DCs and DPTs to be front line providers inasmuch as medical PCPs are woefully ill-trained in MSDs.[18]
Dr. Murphy’s study found that chiropractic offers a non-drug, non-surgical hope to many patients as evident by his patients who had a self-rated improvement of 75.6% overall. “According to our data, there are things [SMT] that can be done to make actual long-term changes.”[19]
Not only does this outcome encourage the use of SMT for this condition, it also raises the question: despite the 75% success rate, these patients still had the pathoanatomy of spinal stenosis, just like patients with degenerative disc disease who used chiropractic care improve.
This is more evidence that the pathoanatomical symptoms are secondary and can be improved by physiological interventions. The paradigm shift in spine care science continues to support the re-focus from pathoanatomical to pathophysiological issues
Dr. Murphy addressed this paradigm shift:
“Clearly the pathoanatomy did not change. We have this discussion frequently in Spine Conference in the neurosurgery department on Monday mornings when I make the point that the spine is capable of handling pathoanatomy as long as the physiology is right (and psychology of course).
“Pathoanatomy only creates the potential for pain. Physiology is what determines whether pain actually occurs or not and psychology determines how much suffering results from that pain.”[20]
This dilemma over the various causes of back pain demands that medical primary care providers understand this complex problem without a bias against chiropractors or a chauvinist attitude about the sanctity of the disc theory, drugs, shots, and spine surgery.
Dr. Murphy says another problem is the prevailing medical bias against DCs:
“Many patients are told not to go to a chiropractor, told that their spine is degenerated and the last thing they want to do is to have someone move it. In my experience, having someone move the spine is the best thing. But the only way to change minds is to come up with credible evidence and substantive argument.”[21]
Dr. Murphy touts the benefit of chiropractic care:
“The advantage we have as nonsurgical spine specialists is when it’s not clear whether a person will respond or not, there’s no harm in giving it a try. The worst thing that can happen is that they don’t respond. With surgery, if you’re not sure whether the person is going to respond or not, it’s a lot harder to just say, ‘Let’s go for it and see what happens.’ You’re making a permanent change in the structure of the spine.”[22]
Issue #4: “You are making people sick”
Is it any wonder that back pain has become the #1 disabling condition in the nation with total costs approaching $300 billion when these “inefficient” medical treatments based on questionable science continue to increase at alarming rates despite the research debunking their premise and questioning their clinical and cost-effectiveness? [23]
This revelation is common knowledge nowadays but ignored by spine surgeons and pain clinics. Sparingly scientific studies and newspaper articles have exposed the overall ineffectiveness of medical spine care that has been called the “poster child of inefficient spine care” by Mark Schoene, editor of THE BACKLETTER, a leading international spine research journal. He was being nice when he said “inefficient.” I would say more often than not it is a case of “deceptive, disabling, and dangerous” spine care.
This opinion is not new. In fact, the famous spine research pioneer, Alf L. Nachemson, MD, PhD, in 1994 accused his spine colleagues of inventing the totally unfounded disease of “disc degeneration.” Nachemson once said to a room full of spine professionals:
“You are violating all the rules of epidemiological science when you name this a disease. You are making people sick…If this is a disease, then this room is full of very sick people.”[24]
Despite his admonition, spine surgeons have ignored his expert opinion and have made billions by deceiving patients despite research showing weak correlation between spine pathoanatomy and pain. At this point it’s simple a matter of ethics, or the lack thereof, by our medical colleagues who perpetuate this unfounded notion that flies in the face of modern research.
Rick Deyo also chided “bad discs” as irrelevant as “finding grey hair” and dubbed them “incidentalomas.”[25] He agrees with Nachemson that “the condition was a non-disease to begin with”:
“And we know that bulging, degenerated, and even herniated discs in the spine are common among healthy people with no symptoms…many of these abnormalities are trivial, harmless, and irrelevant, so they’ve been dubbed ‘incidentalomas’…the patient was destined to get better anyway because the condition was a non-disease.”[26]
Mr. Schoene also suggests “such an important area of medicine has fallen to this level of dysfunction should be a national scandal. In fact, this situation is bringing the United States disrespect internationally.”[27]
Yet, while a leading journalist like Mr. Schoene and spine researchers like Drs. Deyo and Nachemson openly criticizes these medical methods, Becker’s Spine Review, an online newsletter aimed at spine surgeons, takes the opposite position by promoting these controversial methods while ignoring the criticism and evidence-based guidelines altogether other than viewing them as obstacles to circumvent in order to get paid.
Indeed, if one were only to read Becker’s, the paradigm shift in spine care is inconsequential except for the pushback by payers who engaged them in “justification of procedures” and slowly are enforcing the evidence-based guidelines by withholding payments.
For example, in 2011, North Carolina Blue Cross/Blue Shield announced it will no longer pay for spine fusion if the sole criterion is an abnormal disc, which they consider a clinical finding, not a diagnosis.[28]
These insurance companies are basing coverage decisions on the Milliman Care Guidelines, which consider lumbar fusion medically necessary in a few instances:
- spinal fracture
- spinal instability
- neural compression
- repair for dislocation
- abscess or tumors
- spinal tuberculosis
- degenerative scoliosis of greater than 50 degrees with loss of function
- persistent significant radicular pain or weakness or
- persistent neurogenic claudication unresponsive to conservative care.
Further recommendations for spinal fusions to treat stenosis and spondylolysis have specific requirements patients must achieve before surgery is recommended, including failure of at least three months of conservative care.[29]
If BCBS in all 50 states were to enact a similar policy in spine care, imagine the billions of dollars saved and millions of people who would be helped, an issue I’ve written about before, but one ignored by Becker’s and the medical spine cartel.
However, Becker’s recently admitted that several spine device companies have reported a net loss or decreased sales during the third quarter of 2013 when compared with the same period last year.[30]
Perhaps there is light at the end of this fusion tunnel vision as the guidelines and pushback by payers finally make an impact.
Issue #5: Follow the Money or Follow the Evidence?
As chiropractors know only too well, spinal medicine is indeed a “national scandal” with the growing evidence of opioid drug addiction, ineffective and dangerous epidural steroid injections, and spine surgeons “gone wild” doing hundreds of thousands of unnecessary fusions based on the debunked disc theory or irrelevant pathoanatomical diagnostics as we now see with LSS and SIJ cases.[31]
Yet, where is the responsibility and ethical imperative to follow the evidence? Where is the blame for exploiting naïve patients or the penalty for gaming the healthcare system? Asking these questions is as pointless as asking the Bernie Madoff’s and Wall Street bankers to stop scamming the financial system, too.
Keep in mind we are dealing with spine surgeons, the most prosperous with an average salary over $806,000[32] and politically powerful of all MDs as we witnessed when they assassinated the AHCPR after its 1994 guideline #14 on acute low back pain in adults revealed the ugly truth about fusions. [33]
As well, most hospitals want nothing to do with cheap and effective chiropractors treating patients when they can charge $111,662 per spine surgery. As you can conclude, it’s all about money, not philosophical differences, following scientific guidelines, or doing what’s best for the patients.
This dilemma of implementing evidence-based healthcare remains a paradox when research challenges the status quo of economic reality in the American for-profit healthcare.
Yet critics of Obamacare still wonder why government intrusion into this perversely-motivated medical system is necessary. Okay, stop gasping. It’s past time to break up the medical cartel with free enterprise on a level playing field based on evidence, costs, and outcomes. America needs a Teddy Roosevelt to break up the medical monopoly.
And, without a doubt, the spine care business is the best place to start considering back pain is the #1 disabling condition in the world and we chiropractors offer the best treatments for the majority of these cases.
JC Smith, MA, DC, is a 33-year practicing chiropractor, author of The Medical War Against Chiropractors, and he maintains a website, Chiropractors for Fair Journalism.
[1]Testimony before The Institute of Medicine: Committee on Use of CAM by the American Public on Feb. 27, 2003.
[2] Steven P. Cohen, MD, Sacroiliac Joint Pain: A Comprehensive Review of Anatomy, Diagnosis, and Treatment, Anesthesia & Analgesia, November 2005, vol. 101 no. 5: 1440-1453
[3] Washington Post Business, October 28, 2013.
[4] J Silberner, “Surgery May Not Be The Answer To An Aching Back,” All Things Considered, NPR (April 6, 2010)
[5] Anuja Vaidya, Report: Orthopedic Devices Market to Reach $19.2B by 2016, Becker’s Spine Review, December 05, 2013
[6] Elliott Fisher, MD, on the CBS Evening News, “Attacking Rising Health Costs,” June 9, 2006.
[7] Whedon JM, Song Y, Davis MA. Spine J.,Trends in the use and cost of chiropractic spinal manipulation under Medicare Part B., 2013 Jun 14. pii: S1529-9430(13)00521-4. doi: 10.1016/j.spine.2013.05.012.
[8] Washington Post Business, 10/28/2013
[9] SD Boden, DO Davis, TS Dina, NJ Patronas, SW Wiesel, “Abnormal Magnetic-Resonance Scans of the Lumbar Spine in Asymptomatic Subjects: A Prospective Investigation,” J Bone Joint Surg Am. 72 (1990):403–408.
[10] S. Bigos, et al., “Acute Low Back Problems in Adults, Clinical Practice Guideline No. 14,” U.S. Public Health Service, U.S. Dept. of Health and Human Services, AHCPR Pub. No. 95-0642, Rockville, MD: Dec. 1994.
[11] Kim JS et al., Prevalence of disc degeneration in asymptomatic Korean subjects. Part 1: Lumbar spine. Journal of the Korean Neurosurgery Society, 2013; 53(20:31-8.
[12] Lee TH etal., Prevalence of disc degeneration in asymptomatic Korean subjects. Part 2: Cervical spine, Journal of the Korean Neurosurgical Society, 2013; 53(2):31-8.
[13] How common is disc degeneration over the entire spine? The BACKPage, vol. 28, No. 12, December 2013
[14] Bicket MC et al, Epidural injections for spinal pain: A systematic review and meta-analysis evaluating the “control’ injections in randomized control trials, Anesthesiology, 2013; 119:907-31.
[15] Norra MacReady, Epidural Steroids May Increase Fracture Risk, Medscape. Jun 17, 2013.
[16] Centers for Disease Control and Prevention Press Release, CDC Vital Signs: Overdose of Prescription Opioid Pain Relievers—United States, 1999-2008; 2011: www.cdc.gov/media/releases/2011/t1101_presecription_pain_relievers.html .
[17] James N. Weinstein, D.O, et al. Surgical versus Nonsurgical Therapy for Lumbar Spinal Stenosis, N Engl J Med 2008; 358:794-810 February 21, 2008
[18] KB Freedman, J Bernstein, “The Adequacy Of Medical School Education In Musculoskeletal Medicine,” J Bone Joint Surg Am. 80/10 (1998):1421-7
[19] Murphy DR, Hurwitz EL, Gregory AA, Clary R. A non-surgical approach to the management of lumbar spinal stenosis: a prospective observational cohort study. BMC Musculoskelet Disord. 2006;7:16.
[20] Donald Murphy in private communication with JC Smith, July 20, 2012
[21] Chiropractic Approach to Lumbar Spinal Stenosis Part II: Surgery and Treatments By Carol Marleigh Kline, JACA Online editor, MAY‐JUNE 2008
[22] Chiropractic Approach to Lumbar Spinal Stenosis, Part II: Surgery and Treatments
By Carol Marleigh Kline, JACA Online editor
[23] The Burden of Musculoskeletal Diseases in the United States Bone and Joint Decade, Copyright © 2008 by the American Academy of Orthopaedic Surgeons. ISBN 978-0-89203-533-5, pp. 21.
[24] BackLetter, 1994: 9:85-92
[25] Deyo RA. Conservative therapy for low back pain: distinguishing useful from useless therapy. Journal of the American Medical Association, 1983;250:1057-62.
[26]Richard Deyo, MD, PHY and Donald Patrick, PhD, MSPH, Hope or Hype, The obsession with medical advances and the high costs of false promises. 2005 AMACOM books.
[27] US Spine Care System in a State of Continuing Decline?, The BACKLetter, vol. 28, #10, 2012, pp.1
[29] ISASS President Dr. Thomas Errico: Spinal Fusion Coverage Update by Laura Miller, January 28, 2011
[30] Net Losses to Go Around: 11 Recent Spine Device Company Financial Reports, Laura Miller Becker’s Spine Review, December 9, 2013
[31] US Spine Care System in a State of Continuing Decline?, The BACKLetter, vol. 28, #10, 2013, pp.1
[32] “Highest-Paid U.S. Doctors Get Rich with Fusion Surgery Debunked by Studies” by Peter Waldman and David Armstrong, Bloomberg News, Dec. 30, 2010
[33] S. Bigos, et al., “Acute Low Back Problems in Adults, Clinical Practice Guideline No. 14,” U.S. Public Health Service, U.S. Dept. of Health and Human Services, AHCPR Pub. No. 95-0642, Rockville, MD: Dec. 1994.