Home of the Painful
Like mushrooms, patients are kept in the dark about these issues and fed medical manure by MDs who suffer from ‘chirophobia’ or starved by a biased media feigning ignorance of this new research.
To clear this muck from your mind, let me first set the stage to show the enormity of this issue long ignored by the media, an expensive and controversial scandal right under its nose that begs immediate attention.
Unknown to most people, back pain is now the #1 disabling condition in the nation, the military, and in the world, affecting millions of people daily. Musculoskeletal disorders (MSDs) such as low back pain, neck pain, and arthritis affect more than 1.7 billion people worldwide. Low back pain has become the number-one cause of disability worldwide and neck pain the number-four cause.[i]
Before the early 1990s, there was no comprehensive and internally consistent source of information on the global burden of diseases, injuries, and risk factors. To close this gap, the World Bank and the World Health Organization launched the Global Burden of Disease (GBD) Study in 1991.[ii]
Dr. Scott Haldeman, MD, DC, PhD, who chaired the 2000-2010 Bone and Joint Decade Task Force on Neck Pain and Its Associated Disorders, is currently president and CEO of World Spine Care.[iii] “In developing countries, [spinal disorders] can be a death sentence,” said Dr. Haldeman. “We are dealing with a huge, huge problem with very little care available to people in many parts of the world.”
Dr. Haldeman estimates that approximately 70 percent of the populations in developing countries today suffer from back pain and are often given limited treatment options, such as simple naproxen prescriptions for pain, without much follow-up. There are also limited specialists and clinics in many of these regions with proper training to deal with spinal issues.
According Dr. Haldeman: “Spinal disorders have a greater impact than HIV/AIDS, malaria, lower respiratory infections, stroke, breast and lung cancer combined, Alzheimer’s disease, diabetes, depression, or traffic injuries.”[iv]
Not only epidemic in underdeveloped countries, Dr. Haldeman’s study found back pain is virtually inescapable worldwide considering it will also strike most of the 250 million American adults sometime in their lifetime.[v]
- Nearly one-third of adults will suffer daily with low back pain, which equates to 92.5 million people;
- Two-thirds of adults will have a back attack within the year, which equates to 190 million;
- 85 percent or 212.5 million adults will have a severe back attack in their lifetime, and
- 20 percent will describe their pain as severe and crippling.[vi]
Like a Box of Chocolates
When people initially seek help for their ‘back attacks’, it is equivalent to opening Pandora’s Box filled with more than 200 treatment options offered by at least 31 different types of health care providers in the U.S. Patients receive an unpredictable mix of diagnoses, treatments, and ideas about back pain and its causation. This may explain why costs are rising without a corresponding improvement in outcomes.
Dr. Haldeman likened consumers to confused shoppers in a supermarket:
“In this supermarket of over 200 available treatment options for chronic low back pain (CLBP), we are still in the era of caveat emptor (buyer beware)…treatment options appear virtually endless and increasing every year, have strong and vocal advocates, and often limited scientific evidence…Conversely, approaches that have demonstrated only minimal benefit in clinical trials continue to be recommended by proponents…”[vii]
His admission reminds me of Forrest Gump who might have said, “Treatments for back pain is like a box of chocolates—you just never know what you’ll get.”
For the patient suffering from back pain, there are many destinations on the medical railroad, few of which appear to have a happy ending. No passenger on this wild ride knows exactly what the outcome will be or where he will end up. Indeed, the medical ‘quick-fix’ often become a permanent problem.
Considering the huge cost involved for a ride on this medical railroad with 200+ destinations, the consensus of spine researchers and governmental guidelines has startled the medical profession with new findings, new criticisms, and new recommendations for a different track.[viii]
As a chiropractor, I’ve witnessed numerous people being railroaded into drugs, shots, and spine surgeries without given any information that there may be a safer and more effective route to take for their back pain—namely, chiropractic care.
Indeed, we all know people who suffer from failed back surgery, some now addicted to opioid painkillers (medicinal heroin), many people living with disabling back pain, and most of them were not advised to see a chiropractor first as the guidelines now recommend. Due to the politics of medicine in America, many were actually lied to by their primary care physicians or spine surgeon to avoid chiropractic care.
Obviously back pain is an epidemic that has been under-reported by the media as well as allegedly mismanaged by the medical profession to the point where Mark Schoene, associate editor of The Back Letter, an international medical research journal, criticized the ineffective medical spine methods when he declared, “Spinal medicine in the U.S. is a poster child for inefficient care.”[ix]
Elephant in the Room
The current situation in this global pandemic of back pain has not gone unnoticed in the scientific community regarding treatments, costs, and outcomes. The more the investigators look, the more they have concluded the standard medical approach consisting of pain pills, epidural steroid injections, and disc fusions have failed.
Making these ground-breaking discoveries most baffling is its longevity, remaining unnoticed by MDs and unmentioned in the media for over twenty-five years since the first discovery by medical scientists in 1990 that cast strong doubt on the ‘bad disc’ diagnosis for back pain.
This ‘elephant in the room’ looming unnoticed in medical offices and newsrooms concerns a growing consensus in the scientific research journals that upends the very basis of spine fusion surgery for back pain—the ‘bad disc’ premise—a colloquial expression for degenerative disc disease (DDD), but also used interchangeably for slipped, bulging, ruptured, or herniated discs.
However, DDD is now deemed by experts as a ‘non-condition’ due to its high prevalence in pain-free people, but this misdiagnosis is kept alive by spine surgeons and the rest of the medical industrial complex because it is a huge money-maker. Moreover, the public accepts this misdiagnosis because they simply don’t know better.
This controversy came to light once again in November, 2014, when the Mayo Clinic released its review by Waleed Brinjikji, MD, and his colleagues, “Systematic Literature Review of Imaging Features of Spinal Degeneration in Asymptomatic Populations.”[x] This Mayo review found a consensus among 33 MRI studies from around the world that undermines the rationale for fusion surgery based on this ‘bad disc’ idea that is used to lure unsuspecting patients into disc fusion surgery.
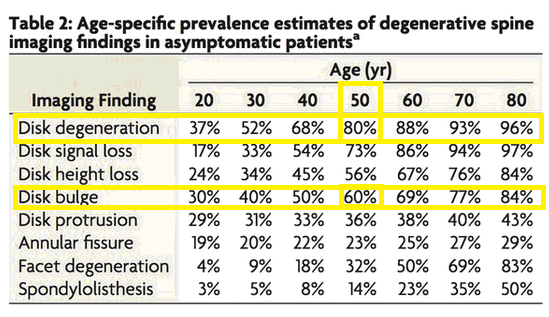
The following list from the Mayo review shows the prevalence of ‘bad discs’ in asymptomatic people of all ages:
- Asymptomatic disc degeneration was exceedingly common and its prevalence increased with age from 37 percent of 20-year-olds to 96 percent of 80-year-olds.
- The prevalence of a disc bulge rose from 30 percent of 20-year-olds to 43 percent of 80-year olds.
- The prevalence of a disc protrusion climbed from 29 percent of 20-year-olds to 43 percent of 80-year-olds.
- The prevalence of asymptomatic annular fissures rose from 19 percent of 20-year-olds to 29 percent of 80-year-olds.
- More than 50 percent of the asymptomatic individuals older than 40 years had a “black disc.” (i.e. disc signal loss on MRI).
- Even more impressively, 86 percent of those aged 60+ years had a black disc.
The Mayo Clinic review was clear that ‘bad discs’ were part of the normal aging process, highly prevalent in people of all ages, often unassociated with pain, and did not alone constitute the need for surgery:
“Our study suggests that imaging findings of degenerative changes such as disc degeneration, disc signal loss, disc height loss, disc protrusion, and facet arthropathy are generally part of the normal aging process rather than pathologic processes requiring intervention.”
According to Mark Schoene, this Mayo study confirms that fusion for DDD may be a medical fraud:
“This is a form of surgery in which the underlying diagnosis has never been validated. There is no diagnostic test—or combination of tests—that can predictably determine whether a patient’s chronic back symptoms stem from degenerative changes in or around the disc or some other anatomic problem. So diagnostic uncertainty shrouds this entire form of fusion surgery.” [xi]
To illustrate the ubiquitous nature of ‘bad discs’ in pain-free people, a study at the Sydney 2000 Olympic Games found these elite athletes had a greater prevalence and greater degree of lumbar disc degeneration than the normal population, yet they were among the best athletes in the world![xii]
Obviously it is easy to find a ‘bad disc’ in most anyone, including elite Olympic athletes, showing these disc changes are not significant and certainly do not require surgery, but this is a huge secret kept from the public by surgeons and a complicit medical media.
The consensus debunking ‘bad discs’ and spine fusion continues to grow. Recently a 2013 study from Korea found as many as 81 percent of patients had a disc herniation, 89 percent had an annular fissure, 95 percent had evidence of nuclear disc degeneration, and none had any pain.[xiii]
Investigators also found a high level of disc abnormalities even among teenagers. “We found close to 25 percent of [10–19 year-olds] have bulging discs at L5/S1…This increases to nearly 30 percent [of 20–29 year-olds].” There were also high levels of disc protrusions in those age groups, yet none had back pain. [xiv]
Another 2013 study from Japan using MRI scans on 975 patients aged 21 to 97 years found the prevalence of disc degeneration over the entire spine was 71 percent in men and 77 percent in women younger than 50 years. The prevalence was more than 90 percent for members of both sexes older than 50 years.[xv] Yet none had back pain.
National Scandal
The issue of low back pain patients misdiagnosed with ‘bad discs’ and mistreated with disc fusions remains a huge financial burden. Its treatment ranks highest among all conditions at nearly $100 billion annually for medical treatment and $300 billion for total costs (lost wages/production, disability compensation).[i]
Hospitalization for spinal fusion surgeries alone creates the largest expenditure of any hospital-based surgery at over $40 billion annually.[ii]
This is an area where adherence to evidence-based guidelines could drastically reduce cost and improve outcomes, yet it fails to gain traction in the mainstream media among medical reporters who inexplicably have ignored this important healthcare breakthrough.
Many surgeries have been deemed unnecessary over the years, but so far disc fusions have remained mysteriously off the radar of the news media that has in the past exposed the rash of tonsillectomies, hysterectomies, Caesarean sections, coronary bypass, angiography, carotid endarterectomy, gastrointestinal tract endoscopy, gastric bypass, hip and knee replacements, just to name a few unnecessary procedures.[iii]
If the truth be known, not only should disc fusions rise to the top of this list of unnecessary surgeries, it should also rank among the most costly and ineffective. More people are victimized with poor outcomes, a lower quality of life, and the cost for disc fusion is far greater than any other surgery despite a growing stream of evidence questioning its clinical and cost-effectiveness.
To say the least, a case can easily be made that medical spine care (consisting of opioid painkillers, epidural steroid injections, disc fusion surgery) is definitely the “poster child” of inefficient spine care, which justifies why Mr. Schoene also warns that “such an important area of medicine has fallen to this level of dysfunction should be a national scandal. In fact, this situation is bringing the United States disrespect internationally.” [iv]
Artificially Sick
Skepticism about spine fusion surgery predates the Mayo review. The history debunking the ‘bad disc’ premise for low back pain formerly took root in 1990 from MRI research by Scott Boden, MD, now Director of the Spine Center at Emory University.[v] His research found ‘bad discs’ in pain-free people confirmed earlier suspicions that herniated, bulging, or degenerated discs may not be the main cause of back pain, thus undermining the reason for the hundreds of thousands of disc fusions done annually.[vi]
Dr. Boden’s study performed MRI scans of sixty-seven asymptomatic patients who had never had low-back pain, sciatica or neurogenic claudication. These scans were interpreted by three neuroradiologists who had no knowledge about the subjects. About one-third of the subjects had a substantial abnormality. In the 60-years-or-older group, the findings were abnormal on about 57 percent of the scans: 36 percent had a herniated nucleus pulposus and 21 percent had spinal stenosis. 35 percent had degenerative or bulging discs.65 Yet none of these patients had any symptoms.
In 1994, Dr. Maureen Jensen, board certified in Diagnostic Radiology, did a follow-up MRI study and came to the same conclusion that the “discovery by MRI of bulges or protrusions in people with low back pain may frequently be coincidental.”[vii]
This controversy has not gone without comment among spine leaders themselves. The renowned godfather of spine research, Alf L. Nachemson, MD, PhD, from Göteborg University in Sweden, accused his spine colleagues of inventing the totally unfounded disease of “disc degeneration.”
Dr. Nachemson chastised a room full of spine surgeons at the International Society for the Study of the Lumbar Spine in Seattle in 1994:
“You are violating all the rules of epidemiological science when you name this a disease…If this is a disease, then this room is full of very sick people.”[viii]
Despite his admonition, spine surgeons continue to ignore these scientific studies and expert opinion while making millions of people ‘artificially sick’ and making billions of dollars deceiving patients despite the accumulating research showing the weak correlation between spine pathoanatomy (such as ‘bad discs’, arthritis, stenosis) and pain.
[i] Peter W. Crownfield, Back Pain Is #1 Cause of Disability Worldwide, Global Burden of Disease 2010 highlights the pressing need to prevent, treat spinal and musculoskeletal disorders. Dynamic Chiropractic – February 15, 2013, Vol. 31, Issue 04
[ii] World Bank. World Development Report 1993 — investing in health: world development indicators. Oxford, United Kingdom: Oxford University Press, 1993
[iii] http://www.worldspinecare.org/
[iv] Scott Haldeman, Analysis of Global Burden of Disease Study 2010 Impact of Spinal and MSK Disorders
[v] The Burden of Musculoskeletal Diseases in the United States Bone and Joint Decade, Copyright © 2008 by the American Academy of Orthopaedic Surgeons. ISBN 978-0-89203-533-5, pp. 21.
[vi] Scott Haldeman DC, MD, PhD, FRCP(C) and Simon Dagenais DC, PhD. A supermarket approach to the evidence-informed management of chronic low back pain. The Spine Journal, vol. 8, Issue 1, January-February 2008, Pages 1-7
[vii] Haldeman, S., Dagenais, S., Evidence-Informed Management of Chronic Low Back Pain Without Surgery, The Spine Journal, January/Feb 2008,Volume 8, Number 1.
[viii] Chapman-Smith D. (2004) Chiropractic Management for Lumbar Disc Herniation, Sept. vol. 18, no. 5, The Chiropractic Report
[ix] The BACKPage editorial vol. 27, No. 11, November 2012.
[x] Brinjikji W, et al., Systematic literature review of imaging features of spinal degeneration in asymptomatic populations, American Journal of Neuroradiology, 2014, prepub ahead of print; www.ajnr.org/content/early/2014/11/27/ajnr.A4173.long.
[xi] Spinal Fusion for DDD a Growth Industry for Two Decades—Despite an Uncertain Evidence Base, BackLetter: April 2015 – Volume 30 – Issue 4 – p 39–41
[xii] A Ong, J Anderson, J Roche, A pilot study of the prevalence of lumbar disc degeneration in elite athletes with lower back pain at the Sydney 2000 Olympic Games, Br J Sports Med 2003;37:263-266 doi:10.1136/bjsm.37.3.263
[xiii] Kim JS et al., Prevalence of disc degeneration in asymptomatic Korean subjects. Part 1: Lumbar spine. Journal of the Korean Neurosurgery Society, 2013; 53(20:31-8.
[xiv] Lee TH etal., Prevalence of disc degeneration in asymptomatic Korean subjects. Part 2: Cervical spine, Journal of the Korean Neurosurgical Society, 2013; 53(2):31-8.
[xv] How common is disc degeneration over the entire spine? The BACKPage, vol. 28, No. 12, December 2013
i] Luo X, Pietrobon R, Sun SX, et al. Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine 2004; 29:79–86
[ii] HCUPnet. Agency for Healthcare Research and Quality. Available at: http://hcupnet.ahrq.gov/HCUPnet.jsp. Accessed October 30, 2014.
[iii] Alexis Black, Unnecessary surgery exposed! Why 60% of all surgeries are medically unjustified and how surgeons exploit patients to generate profits
Friday, October 07, 2005, http://www.naturalnews.com/012291.html#ixzz3VCyMxtqj
[iv] U.S. Spine Care System in a State of Continuing Decline?, The BACKLetter, vol. 28, #10, 2012, pp.1
[v] SD Boden, DO Davis, TS Dina, NJ Patronas, SW Wiesel, “Abnormal Magnetic-Resonance Scans of the Lumbar Spine in Asymptomatic Subjects: A Prospective Investigation,” J Bone Joint Surg Am. 72 (1990):403–408.
[vi] MC Jensen, MN Brant-Zawadzki, N Obuchowski, MT Modic, D Malkasian, and JS Ross, “Magnetic Resonance Imaging of the Lumbar Spine in People without Back Pain,” NEJM, 331/2 (July 14, 1994):69-73
[vii] Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994 Jul 14;331(2):69-73.
[viii] BackLetter, 1994: 9:85-92